JSNA Substance Misuse
Substance Misuse Joint Strategic Needs Assessment
Publication date
This chapter was published in April 2024 and is due to be reviewed by April 2026.
Contents
- Executive summary
- Recommendations
- Introduction
- Scope and methods
- Terminology
- National and local strategic context
- National drug and alcohol use patterns
- Drug and alcohol use in Surrey and its impact
- Drug and Alcohol related hospital admissions and deaths in Surrey
- Drug and alcohol related crime
- Evidence base for interventions
- Prevention, treatment and recovery services in Surrey
- Engagement with treatment
- Stakeholder insights
- Feedback from service users and others affected by drug related harm
- Work taking place to improve the system in Surrey
- Recommendations and rationale for inclusion
- Lead contributors
- Acknowledgements
- Bibliography
Executive Summary
Context
Misuse of drugs and alcohol is a major public health concern with wide-ranging effects on our society including the health, care and financial consequences to individuals, their families, and wider society.
Alcohol and drug use costs the taxpayer millions of pounds every year in dealing with the associated health problems, loss of productivity, children and adult social care costs and drug related crime and disorder. Problematic alcohol and drug use can be a pathway to poverty, lead to family breakdown, crime, debt, homelessness and child neglect.
Investing in a multi-agency response to address drug and alcohol harm has benefits across society. In Surrey, these efforts are delivered by the Combating Drugs Partnership (CDP) which was formed as a result of the government’s 2021 “From harm to hope” drug policy. Surrey’s CDP reports to the Surrey Health and Wellbeing Board (incorporating the Community Safety Board) through its sub-board, the Prevention and Wider Determinants of Health Delivery Board.
The Surrey Health and Wellbeing strategy focuses on Surrey’s Priority Populations (including those with alcohol/drug/serious mental health issues, experiencing homelessness and/or domestic abuse). The Strategy’s Index measures Surrey system’s progress against it.
The term “substance misuse” has been used throughout this JSNA chapter in keeping with the terminology used by the National Institute for Clinical Excellence (NICE), the Office for Health Improvement and Disparities (OHID) and the Office for National Statistics (ONS). However, we recognise that the terminology may continue to evolve in response to increasing understanding of potentially stigmatising language.
The summary of findings below is based on publicly available data, mainly for the financial year 2021/22. Full details are in the main report.
Level of need in the population
In Surrey, the estimated prevalence rate of opiate and /or crack-cocaine use was lower than England and the South-East, but it is estimated that levels of unmet need (the number of people in treatment divided by the estimated prevalence of people using opiates and/or crack cocaine) are higher – Surrey 67.5% and England 57.9%. This data is currently being examined to understand the reasons for this difference.
Of all adults in treatment in Surrey, the most common reported substances were opiates, alcohol, and cannabis. This is slightly different from adults starting treatment in Surrey, where the most commonly reported substances were alcohol, cannabis and cocaine and it reflects that the population of opiate users is ageing. People who use opiates tend to be in treatment longer than most other substances, which reflects the ageing opiate user population.
Nearly a quarter of adults in Surrey reported drinking at increased or higher risk levels (over 14 units of alcohol a week), higher than England levels. In Surrey, levels of alcohol dependence are lower than England, but there has been a gradual increase in numbers in treatment and an increase in hospital related alcohol admissions, mainly for alcohol related liver disease. It is estimated that there are high levels of unmet need for alcohol treatment, at 74%, although this is similar to South-East and England.
For young people, nationally and in Surrey there has been a reduction in people in contact with substance use services. Of those young people in treatment, cannabis remains the most common reported substance with similar levels of use compared to England. This is followed by cocaine, ketamine, and benzodiazepines, all of which had higher rates of reporting than England. A higher proportion of young people commencing treatment for substances in Surrey reported that they had problems with alcohol compared to England. Surrey has a slightly higher proportion of state funded school suspensions and a higher proportion of permanent exclusions due to drugs and alcohol compared to England.
Who is at greater risk?
A range of risk factors can make people more susceptible to drug and alcohol related harm:
- Individual factors, such as mental health, health/disability, trauma, experience of adverse childhood experiences (ACEs), employment /educational /housing /economic status and genetics.
- Interpersonal factors, such as prosocial relationships, peer influences and norms, family structure and functioning.
- Community factors, such as ease of access to drugs, economic and housing opportunity, marginalisation and social isolation /cohesion.
- Institutional factors such as accessibility of drug use services and generic helping services, exclusion, and discrimination.
People who experience severe and multiple disadvantage are in particular at increased risk of drug and alcohol related harm.
Impacts of substance misuse in Surrey
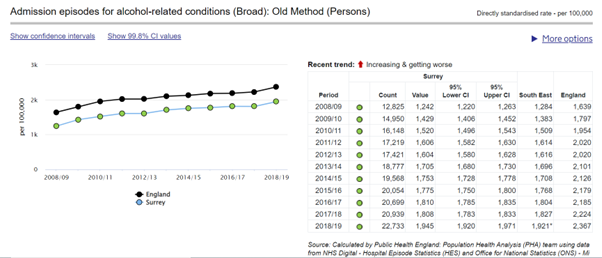
The rate of alcohol related hospital admissions has been increasing over the past ten years in England and Surrey. Overall, the rate of admissions is lower in Surrey than England, however there was a 43% increase in alcohol-related hospital admissions in Surrey between 2008/9 and 2018/19 and some boroughs have higher rates than England. Rates of hospital admissions for alcohol specific conditions for under 18-year-olds in Surrey were higher than England, in particular among girls.
The estimated national cost of the illicit drugs trade is over £19 billion annually. Nearly half of acquisitive crimes are estimated to be associated with drug use. Between 2021-22 over 5,000 drug offences were recorded in Surrey, with cannabis possession the highest drug related offence. This is one of the lowest rates nationally, but data should be treated with caution as it is based on proactive police enforcement activity.
Domestic violence and alcohol are key drivers for homicides. However, it is likely that drugs remain a factor as the scale of offences is not fully known.
The rate of deaths from drug misuse in significantly lower in Surrey than England. The trend over the past ten years has been increasing for England, but with only a slight increase in Surrey. Men and individuals with a diagnosed mental health condition are more at risk.
Evidence base and prevention, treatment and recovery services
Every £1 spent on drug treatment saves £2.50 in costs to society. The substance misuse service system in Surrey includes prevention, treatment and recovery for both children and young people and adults. The aim is to work in an integrated way to ensure a seamless transition from one area to another for the benefit of the clients until they successfully complete their treatment journey. Healthy Surrey provides a full list of all Drug and Alcohol Services (adult and young people) in Surrey. All commissioned services follow National Institute of Clinical Excellence Guidance and Office for Health Improvement & Disparities (OHID)/Public Health England Guidance, these are listed in the main body of the JSNA.
Treatment for substance misuse
A major focus of the national policy drive on drugs is to increase numbers in treatment and reduce unmet needs. In 2021/22 there were 3,842 adults and 209 young people in treatment for drugs and/or alcohol misuse in Surrey. Most adults in treatment were for alcohol or opiate dependency. Waiting times for first treatment interventions in Surrey are good with very few adults waiting more than three weeks. The majority of treatment in Surrey takes place in community settings with only 1% of the adult treatment population attending residential rehabilitation. In line with national trends, since 2009 until the COVID pandemic there had been a decline in Surrey in people aged under 24 years old in structured treatment for substance use. Numbers increased from 2021/2 but have not returned to 2009 levels. All young people in Surrey had community-based treatment.
More men than women are in treatment for drugs and alcohol in Surrey (70% male for drugs, 57% male for alcohol). These gender ratios are similar to those seen in England.
Relative to England, a higher proportion of people in drugs and alcohol treatment in Surrey are of ‘White’ ethnicity; are recorded as having no disability; are in employment; experience no housing problem; are parents who live with their children; are smokers at start of treatment. Mental health needs are high among people entering treatment for drug use, with nearly 80% of females and nearly 70% of males having a mental health need. This difference is also seen among young people with 66% of females and 40% males under 18 years identified with a mental health need.
Adults in both drug and alcohol treatment in Surrey had higher rates of leaving treatment in an unplanned way than England. Compared with England, significantly lower numbers of people successfully engaged in community-based treatment within three weeks of release from prison in Surrey. ‘Successful completion’ of treatment is defined as non-representation within six months of treatment. However, substance misuse is a chronic, relapsing and remitting condition, and those who re-present to treatment may still be on their treatment journey, rather than ‘unsuccessful’. In this context, overall, in 2021/22 Surrey had higher rates of successful completion of treatment for drugs and non-representation within six months than England. However, the rate of successful completions for opiate treatment has declined since 2010 in Surrey and England. Successful completion rates for alcohol and non-opiate treatment in Surrey decreased, whereas in England they increased and a lower proportion of those in treatment in Surrey became abstinent from alcohol.
Themes from stakeholder engagement
Stakeholders such as mental health professionals, housing commissioners, education services, treatment providers, GPs, and the police were engaged by a combination of written feedback and attending meetings/asking for verbal feedback. Themes that emerged from their engagement included:
Prevention: Training and support for non-specialist services such as teachers and police would be helpful. Targeted prevention for particularly priority populations is important – such as looked after children, adult with care experience, and young carers. The increasing normalisation and use of cannabis should be addressed.
Person-centred approach: Building services around people’s needs rather than their diagnoses helps design better services. Outreach and support workers can help people navigate complex systems and avoid non-engagement and help maintain housing. Peer support and workers with lived experience are helpful. Trauma-informed care is important.
Substance misuse services: There is inconsistent investment in alcohol liaison services in acute settings. Residential rehabilitation is not available within county, and there is a lack of detoxification options for people in unstable housing situations. There is a need for more out of hours services, and increased awareness about one stop shop drop ins and warm spaces. Crisis cards with helpline numbers should be widely available.
Mental health: The most complex patients are the most likely to suffer from exclusion criteria when accessing services. The development of more in-reach mental health services could help provide support when people may be more receptive to addressing substance misuse issues.
Criminal Justice: Surrey could improve on test on arrest and use of Drug Rehabilitation Requirements (DRR) and Alcohol Treatment Requirements (ATR), and availability of naloxone. It is important to ensure there is capacity in the system for education and treatment if numbers are increased through proposed introduction of tougher consequences for drug possession.
Recovery: More support is needed for people leaving residential rehabilitation. Housing pathways to meet the needs of high-needs clients and appropriate placements may help prevent failed housing placement. People placed in emergency accommodation out of county may find it difficult to access support and treatment. More partnership with the Department of Work and Pensions could help improve employment opportunities.
Collaboration: Pro-active partnership working across services is important and may help address the challenges of information sharing between agencies. Examples of collaboration included use of shared joint clinic space in community hubs and use of joint local quality assurance guidelines.
Workforce: Frequent staff changes are a concern and may lead to a loss of organisational memory and understanding at a leadership level. More resources to develop the workforce may help address challenges of recruitment, especially of experienced staff within substance misuse services.
People with lived and living experience
The CDP commissioned the public involvement service (Luminus, also home to Healthwatch Surrey) to engage over the period of two years with people with lived and living experience and their families and friends and others affected by drugs and/or alcohol. Findings from the first two quarterly reports are contained in this JSNA and reflect direct feedback from carers, service users, and frontline staff. Findings provide insights into the public’s experiences and perceptions. and will evolve as further reports are collated.
A summary of themes and issues that were highlighted include:
Barriers to access: Stigma and perception of stigma are barriers, lack of awareness that self-referral is possible, perception of rigid processes that don’t work for all.
Communication and signposting: GPs and other frontline health staff may not be aware of services, or may not signpost to services.
Mental health and substance misuse: A perception of lack of support for the trauma that often underlies substance misuse; a perception of not being able to access mental health treatments while using substances; preferring different treatment methods to those on offer.
Continuity of care and establishing trust: Seeing different GPs each time makes it hard to build trust and can be triggering for patients; lack of knowledge of who can help with complex problems; perception of lack of follow-up.
Carers: Difficulties getting loved ones to engage with treatment; perception of lack of support for carers.
Service user feedback: Substance misuse services can be reassuring and can help people who misuse substances become sober.
Recommendations
Recommendations – rationale is set out in the main report
Prevention and early intervention
- Ensure ongoing high profile universal and targeted campaigns on reducing alcohol consumption among adults and young people.
- Embed and strengthen education for professionals and young people on substance use in school, and out of school, settings, including addressing normalisation of cannabis.
- Strengthen pathways between health, social services and drug services to identify and intervene early with vulnerable children and families.
Supporting people into treatment
- Tackle stigma related to substance use, to enable more people to seek treatment and build supportive communities. Encourage CDP partners to undertake stigma training.
- Explore the reasons for Surrey’s higher than England reported rates of unmet need in opiates and crack -cocaine.
- Continue to strengthen pathways between mental health and substance use services to ensure that people are able to access the right care where there is a dual diagnosis.
- Continue to review work by Solutions Research and CDP partners to optimise communication and referral pathways into substance misuse services in Surrey.
- CDP to investigate where there are discrepancies in Criminal Justice Intervention Teams (CJIT) data recording to ensure accurate data reporting.
- Increase engagement by Surrey prison leavers in community drug and alcohol treatment, increasing referrals from the criminal justice system including prisons and probation service. This includes reviewing the needs of male remand prisoners from Surrey in HMP Wandsworth (the main male remand prison for Surrey residents) to ensure effective pathways into treatment and recovery support.
- Optimise the introduction of Police custody ‘test on arrest’ and subsequent referral into treatment.
- Optimise the use of drug rehabilitation and alcohol recovery requirements/programmes within the criminal justice system.
- Understand and optimise referrals for young people from education settings and youth criminal justice settings.
Treatment journey
- Continue to explore reasons for, and reduce the rate of, people leaving treatment in an unplanned way before 12 weeks. Understand why more men than women leave treatment early in an unplanned way, including reviewing access to support.
- Work to understand treatment progress, including why Surrey appears to have a lower rate of successful completions for opiate treatment in adults compared with England.
- Work to understand and increase successful completions for alcohol treatment among adults.
People experiencing multiple disadvantage
- Continue to coproduce and improve engagement with people who experience multiple disadvantage and develop trauma informed practice, including learning from the Changing Futures programme and Multiple Disadvantage JSNA chapter.
- Improve understanding of the Care Act 2014 among organisations who work with vulnerable people such as people with multiple disadvantage and improve understanding of the importance of referring to adult social care for assessment at the earliest opportunity rather than waiting until the person is in crisis.
Wider services
- Continue to monitor the impact of pharmacy closures on harm reduction measures for service users.
- Review the smoking cessation offer to people who use substances as part of new smoking cessation contract with new provider.
Inequalities
- Better understand the interactions between protected characteristics and substance misuse in Surrey.
- Undertake a review to understand unmet need in Surrey, including if ethnic, gender, deprivation and disability differences of those in drug treatment in Surrey represent unmet need/barriers to access.
- Understand and address the higher rate compared to England of alcohol-related liver and/or cardiovascular disease in Runnymede, Spelthorne, Woking and Guildford.
Reducing deaths from drug misuse
- Continue to increase awareness and availability of naloxone within the community.
- Develop a partnership response to drug related deaths through a DARD (drug and alcohol-related deaths review system) approach.
- Undertake a 3-yearly drug-related death audit in partnership with Surrey Coroners’ Office to identify key themes.
- Build our intelligence of drug related deaths and overdoses, including promoting the use of the non-fatal overdose online reporting tool and implementing real-time surveillance of suspected drug-related deaths.
Strengthening recovery – wider determinants
- Review the appropriateness of housing options for people who misuse substances, including people with alcohol-related brain injury. JSNA Housing and Related Support | Surrey-i (surreyi.gov.uk)
- Improve access to accommodation within Surrey alongside treatment for homeless population, especially rough sleepers, to maintain continuity of care.
- Improve employment opportunities, linking employment support and peer support to Job-Centre Plus services, and deliver the roll-out of Individual Placement Support (IPS) from 2024.
- Optimise support for adult carers and young carers of people who misuse substances.
Information sharing and intelligence
- Improve data sharing among partners to understand longer term outcomes of treatment and recovery.
- Develop local outcomes framework to ensure on-going monitoring and review.
- Improve data exchange from ambulance providers via Surrey Office of Data Analytics (SODA) to ensure adequate monitoring of and understanding of naloxone treatment use in the community.
OHID data recommendations
- Include comparison with Chartered Institute of Public Finance and Accountancy (CIPFA) nearest neighbours in commissioning support pack to allow regional comparisons to be drawn.
- Include quality outcomes in addition to process outcomes, which would help understand and evaluate local services.
- Include successful completions and non-representations at 12 and 18 months in addition to the current 6 months. This would give a more nuanced understanding of the patient journey and where to target improvements.
Introduction
The World Health Organisation defines drug misuse as the use of a substance not consistent with legal or medical guidelines. [1] The UK has seen an 80% increase in drug-related deaths since 2012. [2] Drug misuse costs society over £19 billion a year in dealing with associated health problems, lost productivity, adult and children’s social care costs and drug related crime and disorder. [3] Synthetic opioids caused a spike in drug-related deaths in 2023 and are thought to be becoming increasingly prevalent in local drug markets. [4]
According to NICE, problem alcohol use is defined as exceeding the Chief Medical Officer’s low-risk drinking guidelines (a maximum of 14 units a week over at least three days a week, and no alcohol during pregnancy). [5] In England, over 10 million people consume alcohol at levels above this. [6] These people are at increased risk of more than 200 medical conditions associated with alcohol consumption, including various cancers, liver disease, heart disease, and strokes. [6] According to the 2021 Health Survey for England, 28% of men and 15% of women drank at increasing or higher risk levels (over 14 units in the preceding week). [7] In 2017 to 2018 there were over 1.1 million hospital admissions related to alcohol. [6]
Scope and Methods
This needs assessment covers all adults and children and young people living in Surrey and has a particular focus on people in treatment for problematic substance use.
A mixed methods approach was used to inform this needs assessment, including:
- A review of relevant policies, guidance and evidence
- A review of publicly available data, most of which is from the 2023-24 Office for Health Improvement & Disparities’ Adult Drug Commissioning Support Pack [8], Adult Alcohol Commissioning Support Pack [9], and Young People’s Substance Misuse Commissioning Support Pack [10]. These data in turn are mostly obtained from National Drug Treatment Monitoring System data from 1st April 2021 to 31st March 2022.
- For adults, data are available for drugs and alcohol use separately, however for young people, data for drug and alcohol use are usually combined.
- Other sources of data, including police and crime data, are outlined in the national government guidance document: National Combating Drugs Outcomes Framework: supporting metrics and technical guidance (publishing.service.gov.uk) [11]
- Stakeholder insights are included from written and verbal feedback from attending meetings with partners including social care, mental health and other health services, housing, substance misuse service providers and GPs.
- The patient and public lived experience is captured via reports from Luminus.
- Draft recommendations were presented at meetings of CDP subgroups 1, 2, 3, and 4, and to wider stakeholders at a substance use event in September 2023. Their feedback was incorporated into the final recommendations.
Terminology
The term “substance misuse” has been used throughout this JSNA in keeping with the terminology used by the National Institute for Clinical Excellence (NICE), the Office for Health Improvement and Disparities (OHID) and the Office for National Statistics (ONS). However, we recognise that the terminology may continue to evolve in response to increasing understanding of potentially stigmatising language.
National and Local Strategic Context
Dame Carol Black Review
In 2019, Professor Dame Carol Black led a two-part independent review of drugs commissioned by the UK Government. Part one was a broad assessment of the evidence on illegal drug supply into the UK and how criminals meet the demand of users, and part two made specific recommendations for improving prevention, treatment and recovery [12].
National Drug Policy
In December 2021, the Government published a formal response to the Dame Carol Black review. The 10-year drugs plan ‘From Harm to Hope’ [13] has three national strategic priorities:
1. Break drug supply chains
- targeting the ‘middle market’ – breaking the ability of gangs to supply drugs wholesale to neighbourhood dealers.
- rolling up county lines – bringing perpetrators to justice, safeguarding, and supporting victims, and reducing violence and homicide.
- restricting the supply of drugs into prisons – technology and skills to improve security and detection.
2. Deliver a world-class treatment and recovery system
- rebuilding the professional workforce.
- ensuring better integration of services.
- improving access to accommodation alongside treatment.
- improving employment opportunities.
- increasing referrals into treatment in the criminal justice system.
- keeping prisoners engaged in treatment after release.
3. Achieve a generational shift in demand for drugs
- preventing the onset of drug use among children and young people.
- delivering school-based prevention and early intervention.
- supporting young people and families most at risk of substance misuse.
- reducing the demand for drugs among adults.
Local strategic context
Surrey’s Combatting Drugs Partnership (CDP) reports to the Surrey Health and Wellbeing Board through the Prevention and Wider Determinants of Health Delivery Board. The Surrey Health and Wellbeing Strategy focuses on its Priority Populations (including those with alcohol/drug and/or serious mental health issues, experiencing homelessness and /or domestic abuse). There are 14 outcomes (including ‘substance use is low’ and ‘the needs of those experiencing multiple disadvantage are met’) in order to achieve its mission of reducing health inequalities so no one is left behind. The Strategy includes a set of principles for working with communities to support empowered and thriving communities. The Strategy’s Index measures Surrey system’s progress against it.
In June 2022, the Government published guidance for local partners [14] to sit alongside the national ‘From Harm to Hope’ drugs policy outlining the structures and processes through which local partners in England should work together to reduce drug-related harm. Successful delivery of the government’s drugs strategy relies on co-ordinated action across a range of local partners including in enforcement, treatment, recovery and prevention. The guidance sets out in more detail the drugs strategy vision for Combating Drugs Partnerships in each locality.
In May 2023, the guidance for local partners was accompanied by an updated National Combating Drugs Outcomes Framework [11]. This document sets out metrics which form a single mechanism to measure progress across central government and in local areas in tackling misuse of drugs and associated negative outcomes.
The three strategic outcomes are:
- Reducing drug use.
- Reducing drug-related crime.
- Reducing drug-related deaths and harm.
The government aims to deliver these strategic outcomes via intermediate outcomes (also mentioned above in “National Drug Policy” section):
- Reducing drug supply.
- Increasing engagement in treatment.
- Improving recovery outcomes.
Surrey Combating Drugs Partnership
As per Government guidance for local partners, the Surrey Combating Drugs Partnership (CDP) Board was launched in September 2022 to drive the priorities highlighted in the Dame Carol Black Review and national 10-year drugs plan ‘From Harm to Hope’.
In addition, four subgroups have been established to drive forward delivery plans focusing on:
- Breaking drug supply chains;
- World class treatment and recovery system;
- Achieving a generational shift in demand for drugs;
- Reducing alcohol and tobacco related harm.
National drug and alcohol use patterns
National Drug Use patterns
Approximately 1 in 11 adults aged 16 to 59 years (3 million adults) and 1 in 5 adults aged 16 to 24 years (1.1 million adults) reported drug use in the year ending June 2022. There was no change compared with the year ending March 2020. [6]
In the year ending June 2022, 2.7% of adults aged 16 to 59 years and 4.7% of adults aged 16 to 24 years reported Class A drug use; a significant decrease from the year ending March 2020 when this was 3.4% and 7.4%, respectively. [15]
There were no changes in drug use for the majority of individual drugs in the year ending June 2022 compared with the year ending March 2020, except for ecstasy and nitrous oxide; prevalence of ecstasy use fell from 1.4% to 0.7% in adults aged 16 to 59 years and from 4.0% to 1.1% in adults aged 16 to 24 years while prevalence of nitrous oxide use fell from 2.4% to 1.3% for adults aged 16 to 59 years and from 8.7% to 3.9% for adults aged 16 to 24 years. [15]
Decreases in the use of Class A drugs, ecstasy and nitrous oxide may have been a result of the coronavirus (COVID-19) pandemic and government restrictions on social contact. [15]
In the year ending June 2022, 2.6% of adults aged 16 to 59 years reported being frequent users of drugs (using them more than once a month in the past year); this was similar to the year ending March 2020 (2.1%). [15]
Cannabis remains the most used drug in England and Wales since estimates began in 1995. [15] 7.4% and 16.2% of adults aged 16 to 59 years and 16 to 24 years, respectively, reported having used the drug in the last year; a similar level to the year ending March 2020 and the year ending March 2012; however, levels are much lower compared with the year ending December 1995. [15]
In England in 2021, 10% of school pupils thought it was okay to try cannabis to see what it’s like, and 6% thought it was okay to take cannabis once a week. These figures have remained at similar levels since 1999. [16]
Synthetic opioids
Illicit fentanyls and isotonitazene are strong opioids which are more potent than heroin and can be mixed into heroin. They caused spikes in drug-related deaths in England in 2017, 2021 and 2023. [4]
Synthetic opioids are thought to be becoming increasingly prevalent in local drug markets. There are concerns that synthetic opioids may start to be incorporated into non-opioid drugs such as cocaine, benzodiazepines, and synthetic cannabinoids, unknown to people who use these drugs. [4]
National alcohol use patterns
Alcohol misuse is drinking in ways which are harmful, or a dependence on alcohol. Alcohol is a leading cause of premature death in England. 20,970 alcohol related deaths were registered in England in 2021, 38% of which were due to chronic liver disease. [17] Alcohol sales and the amount that people drink increased from the 1980s until reaching a peak in 2008 and declining slightly since then. [6] Some of this decline is due to more adults choosing to be teetotal, as well as fewer young people under the age of 18 drinking alcohol. However, there is large variation in drinking behaviour across different groups. It is largely the people who already tend to drink less that are cutting back, while many of those who are at high risk of health conditions, because they drink heavily, are drinking more now than they did previously. [5]
Risk factors that make people susceptible to drug and alcohol related harm
There are many factors which lead to increased risk of drug related harm. It can be associated with type of drug used (including the forms, routes of administration, amount consumed, context of use, and adulterants) and individual characteristics pertaining to the user (including genetic factors, mental, physical and social morbidities). The harm is also significantly influenced by policy and practice responses to drug use, social /socioeconomic factors, environmental factors, and access to education, employment and recreation. [18]
Specific set of risk factors can make some individuals more vulnerable to the harms associated with drugs. A Drug Misuse Prevention Review has identified following as examples of risk factors [19]:
- Individual: e.g., mental health /well-being, health /disability, trauma, experience of adverse childhood experiences (ACEs), employment /educational /housing /economic status and genetics.
- Interpersonal: e.g., prosocial relationships, peer influences and norms, family structure and functioning.
- Community: e.g., ease of access to drugs, economic and housing opportunity, marginalisation and social isolation /cohesion.
- Institutional: e.g., accessibility of drug use services and generic helping services, exclusion, and discrimination.
- Policy: e.g., housing, employment, education, health and social policy and drugs legislation.
- Macro social system: e.g., population mobility and social inequality.
Who is more at risk? – vulnerable groups
Identification of vulnerable groups can help prioritise resources and ensure we do not discriminate against any groups. However, it is important to note that vulnerability potentially associated with a particular cohort does not automatically lead to vulnerability. Focus solely on the characteristics of specific cohorts can add to the stigma associated with drugs. Therefore, considering risk factors, contexts and behaviours which may make individuals vulnerable to drug use is a more effective approach.
The observed prevalence of past year use (April 2020 to March 2021) of any drug by people aged 16 and over in a Crime Survey of England and Wales was [19]:
- Higher among those unemployed (12.2%) than those economically inactive (7.9%) or employed (5.8%).
- Higher among those who identified as bisexual (11.1%) than those identifying as gay/lesbian (8.8%) or heterosexual (6.5%).
- Higher among those with a disability (8.6%) than among those without (6.1%).
- Higher amongst those in financial difficulty (12.8%) than those financially stable (6.7%).
- Lowest amongst those living in the least deprived areas.
- Higher amongst those who had experienced violence (14.3%) than those who had not (6.3%).
Vulnerability to alcohol misuse can be categorised as societal vulnerability factors or individual vulnerability factors [20].
Societal factors include:
- Alcohol pricing, availability, regulation.
- Drinking context.
- Socio-economic status.
- Culture.
Individual factors include:
- Mental health.
- Homelessness.
- Gender.
- Age.
The following cohorts of people are also at increased risk of engaging in drug and / or alcohol misuse and developing a dependency (including moderate dependency) [18]:
- Lesbian, Gay, Bisexual and Trans (LGBT).
- Black Minority Ethnic Groups.
- Gypsy, Roma, Travellers (GRT).
- Those using prescription or over the counter (OTC) and prescription medicines.
- Those in the Criminal Justice System.
Multiple Disadvantage
People who experience severe and multiple disadvantage are at increased risk of alcohol -related harm including alcohol dependence. People facing multiple disadvantage experience a combination of concurrent problems, and for many their circumstances are shaped by long-term experiences of poverty, deprivation, trauma, abuse, and neglect. Many also face racism, sexism, and homophobia. (About Multiple Disadvantage – MEAM) [21] These inequalities intersect in different ways, manifesting in a combination of experiences including substance use, mental ill health and/or neurodivergent challenges, homelessness, domestic abuse and contact with the criminal justice system. The health inequalities and challenges this population face substantially increases their risk of the early onset of chronic health issues, shortened healthy life expectancy and premature death. [20]
In 2024, Surrey will publish a JSNA chapter on Multiple Disadvantage which will provide significant data and insight into adults, children and young people experiencing multiple and concurrent challenges, including drug and alcohol related need.
Drug and alcohol use in Surrey and its impact
Prevalence of adult opiate and crack cocaine use in Surrey
In Surrey, in 2019/20, the estimated rate of opiate and/or crack cocaine use was 5.0 per 1000 population aged 15 to 64. This was lower than the estimated England rate of 9.5 per 1,000 and the South East rate of 6.6 per 1,000. [8]
For opiates only, Surrey’s estimated prevalence rate was 2.3 per 1000, which was lower than England’s rate of 4.6 per 1000, and the South East’s rate of 2.9 per 1000. For crack-cocaine use, Surrey’s rate was 0.8 per 1000 population, which was lower than England’s rate of 1.3 per 1000, and the South East’s rate of 0.9 per 1000. For both opiates and crack, Surrey’s rate was 1.9 per 1000, England’s rate was 3.6 and the South East region’s rate was 2.8 per 1000. [8]
118 people were identified as homeless with a drug dependency need in Surrey in 2021/22. [22]
Estimated unmet need for Surrey adults who use opiates and crack cocaine
Unmet need is the proportion of estimated opiate and crack cocaine users who are not currently in treatment. In 2021/22, Surrey had higher unmet need than the South East region and England as per table 1 [23]:
Table 1: Unmet need for opiate and crack cocaine users in 2021/22 in Surrey
| Surrey (range), n = prevalence estimate | South East region (range), n = prevalence estimate | England (range), n = prevalence estimate | |
| Opiate and/or crack users | 66.2% (60-71%) N = 3,721 |
58% (54-61%), n = 36,553 | 57.4% (54-60%), n = 341,032 |
| Opiate users only | 64.8% (58-70%) N = 1,712 |
59.7% (56-63%), n = 16,014 | 58.2% (55-61%), n = 164,279 |
| Crack users only | 89.3% (86-91%) N = 571 |
85.6% (84-87%), n = 5,055 | 84.9% (83-86%), n = 47,168 |
| Opiates and crack users | 58.6% (52-64%) N = 1,438 |
47.3% (43-51%), n = 15,484 | 46.3% (43-50%), n = 129,584 |
There are some caveats around these figures on unmet need. People in Surrey who use both opiates and crack cocaine (OCU) have a statistically significantly higher unmet need than the South East region and England. The confidence intervals for the other groups of substance users overlap, meaning the apparent differences between the other groups may be due to chance. The apparent variation in unmet need for OCU between Surrey and the South East and England is being investigated.
Prevalence of hepatitis C in people who inject drugs
In 2021/22, of adults in treatment in Surrey, 21% had a positive hepatitis C antibody test, the same proportion as in England. [24]
Prevalence of other drug use in Surrey adults
The most common substances for all adults in treatment in 2021/22 were opiates, alcohol and cannabis. The most common substances reported by all adults starting treatment in 2021/22 were alcohol, cannabis and cocaine. This reflects known trends in reductions in people starting to use opiates over time, and an ageing population of opiate users.
In 2021/22, the most commonly cited problem substances reported by all adults in treatment for problems with all drugs in Surrey, compared with England can be seen in Table 2:
Table 2: the most commonly cited problem substances reported by all adults in treatment for problems with all drugs in Surrey and England in 2021/22
| Surrey, n (%) | England, n (%) | |
| Opiates | 1,228 (56%) | 140,558 (69%) |
| Alcohol | 769 (35%) | 58,260 (28%) |
| Cannabis | 746 (34%) | 57,355 (28%) |
| Crack cocaine | 661 (30%) | 77,728 (38%) |
| Cocaine | 546 (25%) | 34,837 (17%) |
| Benzodiazepines | 195 (9%) | 14,823 (7%) |
| Amphetamines other than ecstasy | 56 (3%) | 7,400 (4%) |
| Hallucinogens | 50 (2%) | 2,590 (1%) |
| Ecstasy | 24 (1%) | 1,115 (1%) |
| New psychoactive substances | <5 (0%) | 2,331 (1%) |
In 2021/22, the most commonly cited problem substances reported by all adults starting treatment for problems with all drugs in Surrey, compared with England can be seen in Table 3:
Table 3: Most commonly cited problem substances reported by all adults starting treatment for problems with all drugs in Surrey and England, 2021/22
| Surrey, n (%) | England, n (%) | |
| Alcohol | 467 (44%) | 28,541 (37%) |
| Cannabis | 465 (44%) | 28,236 (37%) |
| Cocaine | 396 (38%) | 21,298 (28%) |
| Opiates | 303 (29%) | 33,213 (43%) |
| Crack cocaine | 202 (19%) | 23,543 (31%) |
| Benzodiazepines | 63 (6%) | 3,848 (5%) |
| Hallucinogens | 40 (4%) | 1,666 (2%) |
| Amphetamines other than ecstasy | 33 (3%) | 2,660 (3%) |
| Ecstasy | 19 (2%) | 555 (1%) |
| New psychoactive substances | <5 (0%) | 1,116 (1%) |
Prescription-only and over-the-counter medication use in Surrey adults
In 2021/22, 9% of adults in treatment reported illicit use of prescription only medicines/over the counter medications (POM/OTC), and this figure was also 9% in England. 7% of adults in treatment in Surrey reported non-illicit use of these medications, compared with 4% in England.
Prevalence of alcohol use in Surrey adults
In 2015-2018 (the most recent data available), 23.9% of adults in Surrey reported drinking 14 or more units of alcohol per week, statistically significantly higher than England’s proportion of 22.8%. In 2015-2018, 9.9% of Surrey adults reported alcohol abstinence, statistically significantly lower than 16.2% in England. This may be because Surrey has a lower proportion of ethnicities who are culturally associated with lower alcohol consumption, compared with England as a whole. [25]
There has been a gradual increase in numbers in treatment for alcohol dependence in Surrey from 1,479 in 2018/19 to 2,178 in 2021/22.
From 2008/9 to 2018/19 there was an increase of 43% in alcohol-related hospital admissions in Surrey.
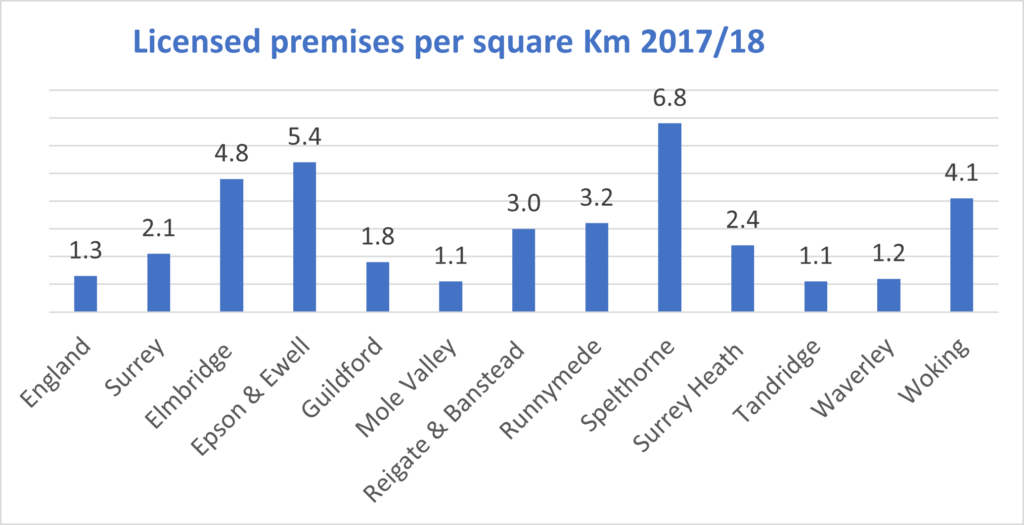
In 2017/18, Spelthorne and Woking were in the top four Surrey boroughs with most licensed premises per square kilometre. Spelthorne and Woking are also two of the three boroughs with the highest rate of hospital admissions for alcohol-related liver disease.
Figure 1: Surrey premises licensed to sell alcohol per square kilometre 2017/18
Estimated unmet need for alcohol use in Surrey adults
In 2021/22, Surrey’s level of unmet need for alcohol treatment was estimated at (73.9%), based on comparing prevalence estimates of adults who have an alcohol dependency problem and numbers in treatment. This is lower compared to unmet need in the South East region at 81.7%, and England’s rate at 80.5% [23]. However, due to overlapping confidence intervals, these rates may not be statistically significantly different.
Prevalence of drug use in Surrey young people
There were 11,326 young people (people under the age of 18) in contact with drug and alcohol services in England between April 2021 and March 2022. This is a 3% increase from the previous year (11,013) but a 54% reduction in the number in treatment since 2008 to 2009 (24,494). Variations in numbers in treatment over the years could indicate wider secular trends of changing substance misuse patterns among younger people, or potential unmet need, or a combination of both and more factors.
In 2021/22 in Surrey, there were 209 people aged under 25 in community structured treatment for young people in Surrey. Cannabis remains the most common reported substance in Surrey young people (79%), which is similar to levels in England (83%).
The next most commonly reported substances were cocaine (22% in Surrey, 12% in England), ketamine (11% in Surrey, 5% in England), benzodiazepines (7% in Surrey, 4% in England), nicotine (7% in Surrey, 11% in England), ecstasy (6% in Surrey, 7% in England), other drugs (6% in Surrey, 3% in England) and other opiates including codeine (2% in Surrey and England).
Prevalence of alcohol use in children and young people in Surrey
In 2021/22, 54% of young people in treatment in Surrey said they had problems with alcohol compared with 47% in England.
In the 28 days prior to commencing treatment for substances, for under-18s in 2021/22, Surrey had higher proportions of heavier drinkers than England as seen in the figure below:
Table 4: Number and proportion of young people (under 18) in treatment by drinking level units for Surrey and England, 2021-22
| Units | Local, n (% of young people) | England, n (% of young people) |
| 0 | 40 (29%) | 4,414 (46%) |
| 1-199 | 82 (59%) | 4,508 (47%) |
| 200-399 | 10 (7%) | 409 (4%) |
| 400-599 | <5 (<5%) | 119 (1%) |
| 600-799 | <5 (<5%) | 43 (0%) |
| 800-999 | 0 (0%) | 24 (0%) |
| 1,000+ | 0 (0%) | 27 (0%) |
| Total | 139 | 954 |
Children looked after with drugs as a factor
Children looked after are a vulnerable group who are at higher risk of substance misuse. Nationally, 3% of young people in community structured substance misuse treatment are children looked after compared with 1% in Surrey (n=8) [26]. This may be a true difference related to a higher proportion of children looked after nationally than in Surrey, or due to data recording/reporting issues.
In Surrey in the year ending 31st March 2022, in factors identified at the end of assessment of a child in need by children’s social care, concerns about drug misuse about the parent were present in 1049 cases and concerns about drug misuse about the child were present in 466 cases. [26]
School exclusions and suspensions that are drug and alcohol related
The school environment is seen as being a protective factor against the uptake of risk-taking behaviours including substance use. Being excluded and/or suspended from school can have a negative effect on young people and increase their vulnerability to problematic substance use and drug-related exploitation.
In Surrey in 2020/21, of the 6,125 total number of state-funded school suspensions, 229 (4%) were related to drugs and alcohol (compared with 3% nationally). [27] Of 84 permanent exclusions from Surrey schools in 2020/21, 9 (11%) were related to drugs and alcohol (compared with 407, or 8% nationally). [27]
Drug and Alcohol related hospital admissions and deaths in Surrey
Hospital admissions due to drug-related poisoning in adults
In 2021/22, hospital admissions for drug-related poisoning were statistically significantly lower in Surrey than in England – 32.3 per 100 000 compared with England’s rate of 42.9 per 100 000. The trend in both Surrey and England is that drug-related poisoning rates have been decreasing since 2018/19.
Hospital admissions due to alcohol in adults
In 2020/21, the directly standardised rate of admission episodes for alcohol-specific conditions in Surrey adults was statistically significantly lower than in England (455 per 100 000 compared with 587 per 100 000). However, some Surrey boroughs have rates above the national average.
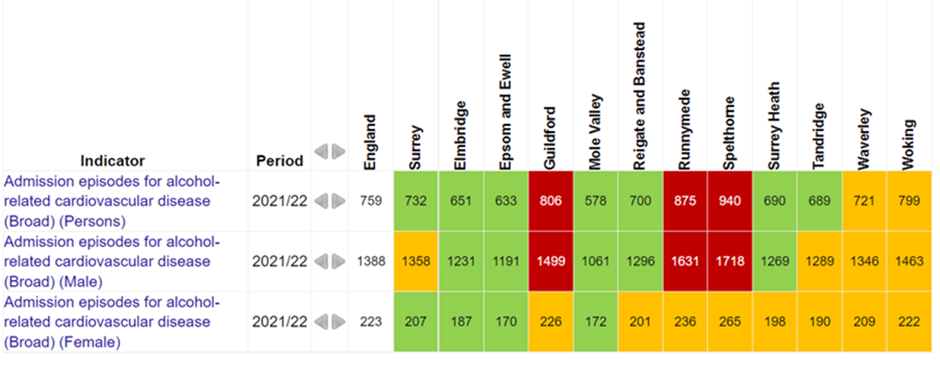
The rate of admission episodes for alcohol-related cardiovascular disease is above the national average in Guildford, Runnymede and Spelthorne, as seen in figure 2:
Figure 2: Admission episodes for alcohol related cardiovascular disease (broad), 2021/22, persons
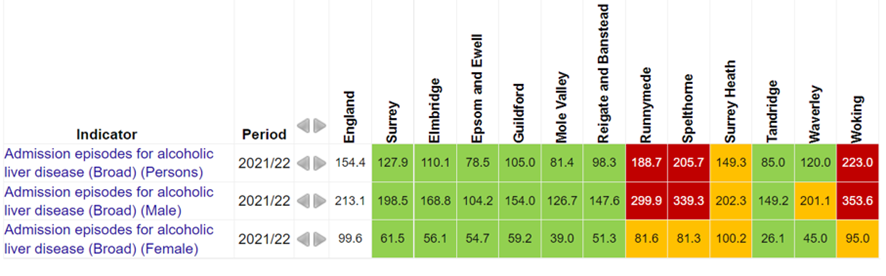
The rate of admission episodes for alcohol-related liver disease is above the national average in Runnymede, Spelthorne and Woking as seen in figure 3:
Figure 3: Admission episodes for alcohol related liver disease (broad), 2021/22, persons
The rate of alcohol-related admission episodes has been increasing over the past ten years in England and Surrey.
Figure 4: Admission episodes for alcohol-related conditions [17]
Hospital admissions due to drug poisoning in young people
In 2018-19 and 2020-21 Surrey’s hospital admissions due to substance misuse (directly standardised rate per 100 000 population of 15-24 year olds) was lower than England but this was not statistically significant (76 per 100 000 in Surrey and 81 per 100 000 in England).
Hospital admissions due to alcohol in young people
In 2018-19 and 2020-21, the directly standardised rate of admission episodes for alcohol-specific conditions in Surrey for people aged < 18 years old was higher than in England, especially in women <18 years old. The overall difference was not statistically significant (33 per 100 000 compared with 29 per 100 000).
Naloxone provision
The use of naloxone is important in reducing opioid-related deaths. A lower proportion of eligible Surrey adults in opiate treatment were issued with naloxone (10%) than adults in England (40%). However, in Surrey there is access to naloxone through community services which may be a preferred collection option for individuals in treatment.
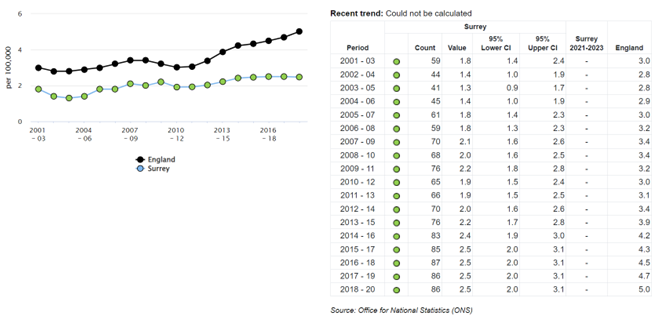
Drug related deaths in adults
Between 2018-2020 there were 86 drug related deaths in Surrey and the directly standardised rate of deaths from drug misuse in 2018-20 was statistically significantly lower than England at 2.5 per 100 000 compared with England’s rate of 5 per 100 000. This trend has been rising in England over the past 10 years and rising slightly in Surrey.
Figure 5: Drug related deaths [28]
Drug-related deaths audit
In 2021, Surrey commissioned a drug-related deaths audit which reviewed 151 drug-related deaths in Surrey between 2017 and 2020. The findings showed that:
- 2/3 of deaths occurred in males.
- The average age of drug related deaths in Surrey residents is 45 years.
- Over 1/3 of individuals lived alone, which is higher than the Surrey average.
- 1/10 were in a relationship.
- 3/10 were unemployed.
- 2/3 of individuals had a diagnosed physical health condition.
- 3/4 individuals had a diagnosed mental health condition.
- Most individuals had more than one substance present at the time of death, and 38% had five or more substances present.
- 3/4 deaths had opiates present.
- Naloxone was only used in 4 of the 91 deaths where opiates were present.
Death by suicide audit
In 2021, a suicide audit was published examining 258 deaths by suicide in Surrey between 2017 and 2020. 57% of people who died by suicide acknowledged either alcohol or substance use before death, mostly long-established alcohol use and/or drug misuse. Only 3% of individuals who died by suicide were in contact with specialist substance misuse services prior to death.
At post-mortem, drugs and/or high levels of alcohol were found in the system of the deceased in 57% of cases, suggesting that half of all cases were under the influence of drugs/alcohol at the moment they took their own life.
Deaths for adults in drug treatment
Surrey’s rate of adults who died within a year of completing drug treatment was 0.8% in 2021/22 compared with England’s rate of 1.3%. The majority of these deaths in Surrey and England were in adults being treated for opiate use. The trend over the past decade has remained around the same level for the past decade. [28]
Alcohol specific deaths in adults
In 2021, alcohol-specific mortality was statistically significantly lower in adults in Surrey than in England (directly standardised rate of 8.1 per 100,000 in Surrey, compared with 13.9 per 100,000). The trend has remained around the same level for the past decade.
Drug and alcohol related crime
The estimated total national cost of the illicit drugs trade, taking into account health and criminal justice costs together, is over £19 billion a year. This is more than double the estimated value of the illicit drugs market itself. [29] 86% of the drug-related costs to individuals and society are concentrated in the markets for heroin and crack cocaine.
National increases in serious violence over recent years are believed to be in part due to drugs. The Children’s Commissioner estimates that 27,000 children in England and Wales identify as gang members. [29]
Neighbourhood crimes
Nearly half of acquisitive crimes (excluding fraud) are estimated to be associated with drug use [30]. In 2021/22, 9,284 neighbourhood crimes were recorded in Surrey, these include domestic burglary, personal robbery, vehicle offences and theft from the person.
Proven reoffending
Surrey’s reoffending rate for January 2021-December 2021 was 20.3%, compared with a rate of 21.6% in England and Wales for the same time-period. [31]
Drug trafficking and possession
Between January 2021 and December 2022, a total of 5,305 drug offences were recorded in Surrey. 4016 (76%) of these were possession offences. 633 (24%) were supply offences. Cannabis possession was the highest drug offence type (3,208, or 80%) followed by cocaine possession (383, or 10%). [32].
Drug offences
Surrey had the 14th lowest rate nationally of drug offences per 10,000 population between June 2019 and March 2022, but this data should be interpreted with caution as this indicator is almost wholly based on proactive police enforcement activity. [33]
Hospital admissions for assault by sharp object
For Surrey for 2020/21, there were 15 hospital admissions aged 0-24 for assault by sharp objects, and 15 hospital admissions for people aged 25+ for assault by sharp objects. [34]
Homicides
There is a correlation between illicit drug use and homicides. From June 2019 to March 2022, Surrey’s homicide rate was 4 per million population, compared with the national average of 10.7 per million population. [33]
The latest data published by ONS’s Homicide Index reports that in the last three years, 28% of homicide suspects and 32% of homicide victims were thought to be under the influence of alcohol and/or illicit drugs at the time of the homicide. 45% of homicide suspects were known to be drug users and 29% to be drug dealers. [33]
Domestic violence and alcohol are key drivers for homicides in Surrey. It is likely that drugs are also a key driver for domestic violence in Surrey, particularly as, since many offences involve survivors who may find it difficult to take part in investigations, the scale of offences is not fully known. [35] A serious violence needs assessment is currently being produced.
Evidence base for interventions
Evidence shows that investing in drug treatment reduces social costs associated with drug misuse and dependence:
- There is evidence that community-based needle and syringe programs are associated with reduced rates of HIV and hepatitis C infection in the target population. [36]
- Opioid substitution treatment (usually methadone or buprenorphine) is associated with reduced drug use, injecting and mortality, as well as reduced crime and reduced offending proportionate to the time spent in treatment. [36]
- Specialist drug treatment services in England are associated with reductions in offending. [36]
- The evidence for psychosocial intervention treatments is more mixed. [36]
- It is estimated that the net benefit-cost ratio is £2.5 in cost savings for every £1 spent on treatment. [36]
The evidence-based interventions for alcohol use disorders encompass a range of strategies proven effective for reducing alcohol related harm. The interventions include:
- The Alcohol Use Disorder Identification Test (AUDIT) is the gold standard screening tool used for identifying individuals at risk of alcohol use disorders. This is a cost-effective method for early detection of alcohol-related problems and can be applied in various settings, including healthcare. Studies indicate that using AUDIT for screening and subsequent intervention can lead to significant improvements in patient’s alcohol consumption patterns and overall health outcomes.
- Identification and Brief Advice (IBA and Extended Brief Advice (EBA) are evidence-based interventions that show efficacy in addressing alcohol use disorders. IBA typically involves a short screening using tools like AUDIT, followed by brief, structured advice on reducing alcohol consumption. This approach is particularly effective in primary care and community settings. EBA extends this model by providing more in-depth counseling and follow-up sessions. Studies have shown that both IBA and EBA can lead to significant reduction in alcohol consumption among moderate-risk drinkers.
- Identification and brief advice in primary care can save the NHS up to £27 per patient, per year.
- Small-scale evaluations show that assertive approaches working with High Impact Complex Drinkers can deliver reductions in service use, savings to the healthcare system and reducing alcohol related harm.
- At the policy level, minimum unit pricing, taxation and regulation of the availability of alcohol, have proven to be effective interventions reducing alcohol related harm.
- Alcohol public awareness campaigns and educational programmes are crucial in raising awareness, changing behaviours, and ultimately reducing alcohol related harm in the community.
- Young people’s drug and alcohol interventions result in £4.3 millions health savings and £100 millions crime benefits per year.
- Alcohol treatment reflects a return on investment of £3 for every pound invested.
Commissioned services follow best practice and guidance as detailed in the following NICE guidelines:
Drug misuse prevention: targeted interventions NICE guideline [NG64] Published: 22 February 2017 [37]
Drug misuse in over 16s: opioid detoxification Clinical guideline [CG52] Published: 25 July 2007 [38]
Drug misuse in over 16s: psychosocial interventions Clinical guideline [CG51] Published: 25 July 2007 [39]
Coexisting severe mental illness and substance misuse: community health and social care services NICE guideline [NG58] Published: 30 November 2016 [40]
Drug use disorders in adults Quality standard [QS23] Published: 19 November 2012 [41]
Alcohol-use disorders: diagnosis, assessment and management of harmful drinking (high-risk drinking) and alcohol dependence Clinical guideline [CG115] Published: 23 February 2011 [42]
Alcohol-use disorders: prevention Public health guideline [PH24] Published: 02 June 2010 [43]
Alcohol-use disorders: diagnosis and management of physical complications Clinical guideline [CG100] Published: 02 June 2010 Last updated: 12 April 2017 [44]
Alcohol and drug misuse prevention and treatment guidance Office for Health Improvement and Disparities Published 20 December 2017 Last updated 7 March 2023 [45]
Drug misuse and dependence: UK guidelines on clinical management Department of Health and Social Care Published 14 July 2017 Last updated 15 December 2017 [46]
Service user involvement: A guide for drug and alcohol commissioners, providers and service users Public Health England 2015 [47]
New psychoactive substances (NPS) in prisons – A toolkit for Prison Staff Public Health England 2016 [48]
Substance misuse services for men who have sex with men involved in chemsex Public Health England 2015 [49]
Prevention, treatment and recovery services in Surrey
Prevention services for adults
Surrey has a range of both primary and secondary prevention substance misuse interventions including:
Primary prevention
- Surrey residents have free access to a screening online tool (Drink Coach) which uses the AUDIT score to categorise people into varying levels of risk of harm from alcohol Alcohol Test | DrinkCoach — DrinkCoach.
- Surrey County Council promotes the following campaigns: Dry January, Alcohol awareness week in July and Sober October.
- Surrey County Council has mapped Surrey neighbourhoods with high rates of alcohol-related admissions, and provides focused information to these neighbourhoods about the Healthy Surrey website, and signposts to services.
- Adopting the Making Every Contact Count (MECC) approach, including training the wider workforce including health and care providers, criminal justice, probation, job centres, adult social care to identify individuals at risk of harm from alcohol using the AUDIT score and signposting them to help.
Secondary prevention
- Harm-reduction approaches within community and outreach settings (as people who engage in treatment have a lower risk of drug related death).
- A help line for individuals seeking advice about drug and alcohol use.
- Naloxone provision.
- Surrey County Council commissions workers who are integrated into different services such as probation, and Women’s Support Centre to identify individuals at an earlier stage in their drug and alcohol use to prevent long term harm.
- Surrey substance misuse treatment services provide training for professionals in housing, police and health, to identify individuals who would benefit from help and provide brief interventions.
- Surrey County Council supports the Surrey Liver Health Check Programme identify people at early stages of liver disease and signposts to services.
- Surrey County Council has commissioned training sessions via Alcohol Change UK for alcohol treatment workers about various issues affecting people who misuse alcohol.
Community drug and alcohol services for adults
i-access is the main service commissioned by Surrey Public Health for adults aged over 18 years who use drugs and/or alcohol. It is led by the Surrey and Borders Partnership NHS Foundation Trust (SABP) who subcontract VIA (formerly known as Westminster Drug Project) for certain elements of the contract.
i-access provide both pharmacological and psycho-social treatment. i-access is co-located with Adult Social Care Substance Misuse Team, who provide assessment under the Care Act, lead on Adult Safeguarding and assess for suitability for residential rehabilitation. Surrey Public Health and Adult Social Care each funds part of rehabilitation.
i-access services include support groups for:
- Abstinence preparation.
- Non abstinence.
- Peer mentoring.
- Recovery café.
- Relapse prevention.
- SMART recovery.
- Women’s group.
- Managing anxiety group.
- Alcohol education group.
i-access services include detoxification services for home detoxification and community detoxification (sometimes known as “ambulatory detoxification”). i-access can refer into inpatient detoxification if appropriate.
Adult Social Care Substance Misuse Team
In Surrey, there is a standalone Substance Misuse Social Care Team which works in partnership with health substance misuse treatment delivery (i-access). The Substance Misuse Social Care Team is county wide and comes under the umbrella of Specialist Mental Health Services and is directly accountable to Surrey County Council Adult Services. ASC Substance Misuse have separate responsibilities but are collocated and work collaboratively with i-access. They also receive referrals through Adult Social Care and work with service users who may not be receiving support from treatment services.
Within this co-located system, health undertake clinical work and treatment whilst social care focus on social care, such as:
- Care Act (2014) compliance; Safeguarding; Social care assessments (Care Act 2014) and reviews; Carers (Care Act 2014); Support planning and provision of packages of care to support care and support needs; Crisis intervention; Mental capacity assessment; Wellbeing and prevention.
- Social Care manage the rehabilitation pathway via assessment, provision and support for rehabilitation programs through our social care processes and RAP (Rehabilitation Assurance Panel).
- Offer joint working and training to mental health, hospital and general locality social care services.
- Embedded in the Surrey County Council Health and Wellbeing Multiple Disadvantage agenda and from this they offer wider training in relation to social care services.
Surrey Public Health also commission services that are part of the long-term recovery agenda. These services include:
- Telephone helpline – free and confidential service for those experiencing problems with substance use and their families (Surrey Drug and Alcohol Care)
- Telephone counselling for those who have experienced a non-fatal overdose, and those bereaved due to a drug-related death (Surrey Drug and Alcohol Care)
- Supported accommodation for adults in recovery from drugs and/or alcohol (Transform Housing and HomeGroup)
- Recovery workers to work specifically with women at risk of engagement with the criminal justice system, based within Surrey’s Women’s Support Centre
- Cuckooing service (co-commissioned with the Office of the Police and Crime Commissioner), supporting vulnerable adults at risk of exploitation due to drug dealing (Catalyst)
- Naloxone and needle exchange provision and training, offering support to organisations working with vulnerable adults (Guildford Action)
- Advocacy service to support those engaging in treatment for substance use (POhWER)
- Public Involvement service for those impacted by substance use (Luminus)
Community services for people experiencing multiple disadvantage
Lankelly Chase’s report, ‘Hard Edges: Mapping Severe and Multiple Disadvantage in England’ estimates that each year, over a quarter of a million people in England have contact with at least two out of three of the homelessness, substance use and/or criminal justice systems, and at least 58,000 people have contact with all three. Multiple disadvantage refers to people experiencing three or more challenges concurrently. In the current uncertain climate, the severity and complexity of multiple disadvantage is increasing; and responding at crisis point is harder to resolve someone’s needs and more expensive for the system.
For people experiencing multiple disadvantage, substance use and mental health needs are identified as two of the primary needs. Research suggests that accessing the right support, maintaining support, being discharged from services for missing appointments or for attending appointments while intoxicated, and not being able to access mental health support until having addressed substance use issues are some of the key barriers faced by people experiencing more than one challenge at the same time (“co-occurring conditions” or “dual diagnosis”). [50]
Co-design of services with people with lived experiences helps to challenge assumptions and identify barriers and helps change services and the system to work better for people experiencing multiple disadvantage. Surrey is implementing this in the form of the Changing Futures programme.
Some Surrey residents who experience multiple disadvantage are receiving support from Changing Futures.
The majority (93%) of Changing Futures beneficiaries have experienced mental health issues, and 85% report drug or alcohol use, (figures are based on 1552 national sample). The Bridge the Gap service is funded to support 90 people experiencing severe multiple disadvantage. However, engagement from the wider partnership including service providers and health and social care partners indicates there could be as many as 3,000 people experiencing multiple disadvantage in Surrey, signifying a potential shortfall in provision to meet the current need.
The Bridge the Gap Alliance offers person-centred key-worker support to people experiencing multiple disadvantage, which includes people who use drugs and alcohol. The Alliance is made up of a group of third-sector providers that have partnered to provide a specialist offer of support, and they include Oakleaf, Catalyst, Rentstart, The Hope Hub, Surrey Domestic Abuse Partnership, Guildford Action, Surrey and Borders Partnership, The Richmond fellowship amongst others. [51]
Harm reduction in Surrey
Surrey Public Health commissions needle exchange services via Community Pharmacy. There are two specialised needle exchange services – Guildford Action which is a charity and Woking Exchange run by i-access. In addition, needle exchange and naloxone are also available through other community sites including York Road Project, Catalyst and the Hepatitis C Operational Delivery Network. Some pharmacies have also signed up to provide naloxone in injectable and nasal inhalation form.
There is currently a trial with Guildford Action to provide inhalation kits to reduce the risk of blood borne virus transmission between people who share pipes to take crack cocaine and if successful this will be rolled out to community pharmacies in Surrey.
Nine pharmacies closed in the Surrey Heartlands and Frimley Integrated Care Board areas between the 22nd April and the 13th June 2023, and two additional pharmacies closed within a one-mile of the Surrey area. [52] It is reported by i-access and Luminus that pharmacy closures are likely to negatively impact on service users as individuals may have to travel further and at more expense to access opiate substitute treatment and clean needles. This may result in reduced engagement with these interventions.
Alcohol interventions for adults
Alcohol liaison teams (ALTs) respond to patients presenting acutely to in- or out-patient clinical settings who are assessed as having an alcohol related problem. Their role is to prevent inappropriate admissions and redirect to community alcohol treatment services. Surrey Public Health coordinate with Surrey Heartlands ICS alcohol liaison teams as part of the Combating Drugs Partnership subgroup 4, to reduce alcohol related risks.
Four Surrey trusts currently provide alcohol liaison services, with the biggest being Royal Surrey Hospital which provides services five days a week during working hours. Ashford and St Peters have a smaller team of three alcohol liaison nurses. East Surrey and Frimley Hospital also have smaller alcohol liaison services. Epsom Hospital does not currently provide any alcohol liaison services.
Once the alcohol liaison team have identified inpatients at increased risk from alcohol or alcohol dependency, they refer them to i-access where they are assessed and receive an offer of a treatment pathway appropriate for their needs.
Surrey Public Health and the Office of the Police and Crime Commissioner co-commission the High Impact Complex Drinkers (HICD) service. This is provided by VIA who work on a more one-to-one basis with individuals whose drinking is high-risk, and who are not engaged with services. These individuals may be high attenders at A&E or have complex health and/or social care needs.
Surrey Public Health provides funding for training for professionals (from many agencies including NHS, Surrey Police, voluntary organisations) and is producing a making every contact count (MECC)-based alcohol toolkit.
As part of the CDP, Surrey Public Health leads communication campaigns to increase awareness of alcohol-related risks to the wider population. This includes working with partners to promote the main campaigns – alcohol awareness week, dry January, an alcohol-free month – and encourage the uptake of online alcohol tests provided by DrinkCoach.
Prison drug and alcohol services for adults
NHS England commissions drug and alcohol treatment services for people who are in prison. Surrey has five prisons. Drug and alcohol treatment are provided by Forward Trust:
NHS England undertook health needs assessments for residents of Surrey prisons in 2021.
Prevention services for young people
Surrey County Council uses a Healthy Schools approach and commissions materials including education toolkits to support the delivery of PSHE in schools to educate children and young people about substance misuse.
Surrey County Council commissions workers who are integrated into different services such as youth offending, CAMHS and the Surrey Police Child Exploitation and Missing Unit (CEMU).
Catch-22 provide prevention and early intervention work in schools and to Surrey’s youth provision (youth clubs, targeted youth work).
Drugs and alcohol services for young people
The main drug and alcohol service Surrey Public Health commissions for young people is Catch-22 which is a social enterprise for children and young people aged from 11 years up to the age of 25. Within the past year, Surrey Public Health has commissioned Catch-22 to provide dedicated substance use posts based within the Youth Justice Service (YJS) for: young people age <18 years; 18-24 year olds in probation; working directly with CAMHS; and working within the Child Exploitation and Missing Unit (CEMU).
As well as treatment, Catch-22 also engage with schools and deliver training in substance use for all professionals working with young people, including foster carers.
Catch-22 has an additional service called Music to my Ears which engages with young people at risk of becoming involved in the criminal justice system, many of whom use drugs and alcohol.
Amber is a charity which has four supported housing centres in Kent, Surrey, Wiltshire and Devon accepting young people aged 16-30, from across the country. Surrey Public Health commissions two beds for young adults (17-25 years). They tend to be young people who are engaged with Catch-22 and who need assistance in engaging with education, employment or training.
Adults in drug and alcohol treatment – overview
In 2021/22, there were 3,842 adults in drug treatment in Surrey. These comprised 1,228 being treated for opiates, 428 for non-opiates only, 1,657 alcohol only, and 529 non opiate and alcohol.
Young people in drug and alcohol treatment – overview
In 2021/22, 209 young people aged under 18 and 18-24 in young people’s services were in treatment for drugs and alcohol use in Surrey.
Routes into treatment (referral sources)
Routes into adult drug treatment
For adults starting drug treatment in 2021-22 in Surrey, when compared with England, a lower proportion were self-referrals (51% in Surrey vs 57% in England), and criminal justice system referrals (10% vs 17%). A higher proportion were referred by health care or social services – GP (9% vs 4%), hospital/A&E (7% vs 2%), and social services (5% vs 3%). This could indicate that Surrey services are more effective at reaching clients than services in England, such that health and social care services detect and refer patients on appropriately, meaning the need for self-referral or criminal justice referral is lower. Or it could indicate that patients in Surrey do not self-refer at any early enough time and are therefore only referred in for treatment once they have reached a worse condition that required them to seek medical help.
Routes into adult alcohol treatment
For adults starting alcohol treatment in 2021/22 in Surrey, compared with England, a lower proportion were self-referrals (52% in Surrey vs 61% in England), and criminal justice system referrals (4% vs 6%). A higher proportion were referred by health care or social services – GP (16% vs 8%), hospital/A&E (11% vs 7%), and social services (4% vs 3%). This could indicate that Surrey services are more effective at reaching clients than services in England, such that health and social care services detect and refer patients on appropriately, meaning the need for self-referral or criminal justice referral is lower. Health-service referrals are encouraged as formal referrals are trackable, whereas if a person is signposted to self-refer the original referrer will never know if the service ever saw the patient. Or the lower rate of self-referrals in Surrey than England could indicate that patients in Surrey do not self-refer at any early enough time and are therefore only referred in for treatment once they have reached a worse condition that required them to seek medical help.
Routes into young people’s drug and alcohol treatment
In 2021/22, a lower proportion of Surrey under 18s were referred into treatment via education (15%) compared with England (31%) and youth criminal justice system (3% in Surrey and 18% in England). A greater proportion of Surrey than England’s under 18s were referred in by social care (32% vs 25%), self, family and friends (19% vs 11%), and health services (28% vs 14%).
Waiting times for treatment
Waiting times for drug treatment for adults
In 2021/22, 99% of adults waited < 3 weeks for treatment, 1% waited 3-6 weeks, and 0% waited >6 weeks. This is slightly better than England where 98% of adults waited < 3 weeks, 1% waited 3-6 weeks, and 1% waited >6 weeks.
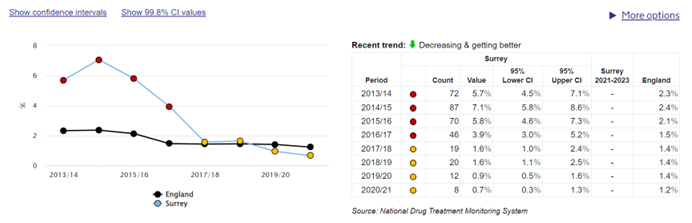
The trend for Surrey has improved over the past decade and continues to improve as per figure 6 below.
Figure 6: proportion waiting more than three weeks for drug treatment [62]
Waiting times for alcohol treatment for adults
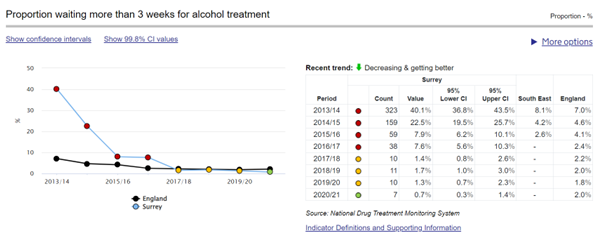
Waiting times for first interventions for Surrey has significantly improved since 2014/15. In 2014/2015, 22.5% of clients waited longer than three weeks to receive treatment. In 2021/22, 99% of all interventions started withing 3 weeks which is similar to England (98%).
Figure 7: Proportion waiting more than 3 weeks for alcohol treatment [62]
Waiting times for drugs and alcohol treatment for children and young adults
There is no national target for waiting times for young people but there is a local target where there should be no waiting time for children and young adults as Catch22 make contact and allocate a worker within 24-48 hours of referral, with an initial appointment offered within 5 working days, and the aim of first interventions to be complete within three weeks of receipt of referral.
Engagement with treatment
Engagement with drug services for adults
In 2021/22, adults in drugs treatment in Surrey had a higher rate of leaving treatment in an unplanned way than England (30% in Surrey, compared with 18% in England).
Proportion of adults who attended residential rehabilitation
In 2021/22, in Surrey, 12 adults (1% of the treatment population) attended residential rehabilitation. This compares with England’s figures of 3094 adults (2% of the treatment population).
Adult inpatient uptake
In 2021/22, 78 adults (4%) in Surrey received care in an inpatient unit during their treatment journey. This compares with 5493 adults (3%) in England.
Number in adult drug and alcohol treatment in prisons and secure settings
In England, in 2021/22, there were 45 096 people in drug and alcohol treatment in prisons and secure settings, a 3% rise compared with the previous year. [53]
Proportion of adults in prison starting treatment within three weeks of arrival
62% of adults starting treatment who were taken directly into custody from the community started treatment immediately on arrival in secure settings. 88% started within 3 weeks of arrival. 38% of people transferring from another secure settings took over 3 weeks to start treatment. These people may have developed drug problems in custody or decided they want to access treatment before their release, rather than being people who have a break in their treatment when they transfer from one prison to another. [24]
Prison services continuity of care
In 2021/22, significantly lower numbers of people successfully engaged in community based structured treatment within three weeks of release from prison in Surrey (24%) compared to England (37%). However, these figures were audited locally by the service provider in conjunction with the prisons and are thought to be due to data-recording error. Work is being undertaken to improve accurate data recording.
NHS England undertook health needs assessments for residents of Surrey prisons in 2021.
Criminal justice system involvement of those in adult drug and alcohol treatment
In 2021/22, the number of adults with prior convictions in the two-years preceding alcohol-only treatment was lower in Surrey (16%) than England (21%).
In 2021/22, no adults in the criminal justice system in Surrey were in alcohol-only treatment, compared with 3% in England. However, this may be data artefact due to low numbers.
Community Sentence Treatment Requirements (CSTRs) are community sentences issued by courts where the offender has consented to complete treatment for mental health problems, drug and/or alcohol misuse problems. Treatments are arranged as part of the sentence imposed.
These can last a maximum of three years as part of a Community Order and two years as part of a Suspended Sentence Order.
There are three types of CSTR:
- Mental health treatment requirements (MHTR).
- Drug rehabilitation requirements (DRR).
- Alcohol treatment requirements (ATR).
For dual diagnosis it is possible for the court to impose both an MHTR with either an ATR or DRR. It is not possible to have an ATR/DRR as a combined order. As the treatment provider is the same for people on ATRs and DRRs, if someone needed both, it is likely that they would receive a DRR.
Between April 2021 and March 2022 in Surrey, Surrey probation data show that 54 people were on a DRR (35 people with a Community Order and 19 people with a Suspended Sentence Order were on a DRR).
For the same time period in Surrey, 79 people were on an ATR (52 people with a Community Order and 27 people with a Suspended Sentence Order were on an ATR).
However, NDTMS data show that in 2021/22, the proportion of adult criminal justice system referrals that had a DRR was lower in Surrey (0%) than England (5%), and the proportion with an ATR was also lower in Surrey (0%) than England (3%).
This discrepancy between Surrey probation data and NDTMS needs further investigation to ensure we have accurate data.
NDTMS data for 2021/22 show that the proportion of arrest referrals was lower (4% in Surrey vs 10% in England), which may improve after the recent introduction in Surrey of “drug test on arrest”. The proportion of prison referrals was lower in Surrey than England (42% vs 51%), which may possibly be due to data recording error, which is being addressed. The proportion of liaison and diversion and probation referrals was higher in Surrey than England (10% vs 2%, and 44% vs 29% respectively).
In 2021/22, compared with England, Surrey prison-leavers had lower rates of engagement in alcohol treatment (14% vs 6%) after leaving prison. However, similarly to the section above on post-prison engagement with drugs treatment, this may be due to data-recording error. Work is being undertaken to improve accurate data recording.
Engagement with alcohol services for adults
In 2021/22, adults in alcohol treatment in Surrey had a higher rate of leaving treatment in an unplanned way before 12 weeks than England, and males were more likely to leave treatment early than females. Figures for Surrey were 34% for males and 29% for females compared with England’s 15% for males and 12% for females.
Engagement with drug and alcohol services for young people
The number of under 18s and 18-24 year olds accessing young people’s structured treatment in Surrey increased in 2021/22, following a dip during the lockdown period in 2020/21 and a decrease prior to that. Numbers have continued to rise in 2022/23, with 239 under 18s accessing structured treatment and an additional 80 receiving non-structured support. However, similar to the national trend, the local number of young people accessing treatment in Surrey still has not returned to the level in 2009/10. There are a number of reasons why this may be the case, as the number of young people seen in Surrey for a shorter intervention increased during this time, meaning that young people did not require a structured intervention and were perhaps seen at an earlier stage of their drug use before it developed further.
100% of young people under the age of 18 in Surrey in 2021/22 (146 young people) were being treated in the community, with nobody being treated in residential rehabilitation or inpatient settings. This is broadly similar to England.
Criminal justice system involvement of those in young people’s drug and alcohol treatment
In 2021, Surrey had a statistically significantly lower rate of first time entrants aged under 18 to the criminal justice system than England (crude rate 81 per 100 000 in Surrey compared with 147 per 100 000 in England).
In 2021/22, a lower proportion of Surrey under 18s were referred into treatment via the youth criminal justice system compared to England (3% in Surrey and 18% in England). However, this data may not be reliable as young people may be referred into treatment by social care but not be identified as being engaged with the youth justice system. This should change now that there is an integrated Catch-22/youth justice system worker.
Number in young people’s drug and alcohol treatment in prisons and secure settings
In England, in 2021/22, there were 553 young people in drugs and alcohol treatment in prisons and secure settings, a 17% reduction compared with the previous year. [53]
Features of those in treatment
Demographic groups
Ethnicity of those in adult drug treatment
In 2021/22, 88% of those presenting to adult treatment in Surrey were White British, which is higher than the White British population of Surrey which is 76.6%. 4% of those presenting for adult treatment were Other White, though Other White residents comprise 8.9% of the Surrey population. The number of clients starting treatment from other ethnic backgrounds, such as White Irish (1%), White and Black Caribbean (1%), Pakistani (1%), White and Asian (1%), and Other (1%) was relatively low.
The proportion of new presentations from people of a White and Black Caribbean ethnicity was 2% which is higher than the 1.0% of the Surrey population whose ethnicity is mixed. The proportion of new presentations for people of Caribbean ethnicity was 2%, which is higher than the 1.1% of the Surrey population who report their ethnicity as Black British, Caribbean, or African.
Ethnicity of those in adult alcohol treatment
In 2021/22, 89% of new presentations for alcohol only treatment in Surrey were White British which is higher than the White British population of Surrey (which is 76.6%), and higher than proportion of 82% in England. This could be because alcohol intake is lower in certain ethnic groups compared with the White British population, or it could represent unmet need if people from ethnic minorities would benefit from treatment but are not being detected by current methods.
Ethnicity of those in young people’s drug and alcohol treatment
In 2021/22, 71% of young people (under 18) engaged in structured treatment in Surrey identified themselves as being White, 5% as White Other and 3% White and Black Caribbean and Other Mixed. 8% were identified as Asian / Other Asian / White and Asian.
Age of Surrey residents
The age distribution in Surrey is older than England and Wales as a whole, with more individuals aged over 40 years and fewer aged 0-4 years old and 20-40 years old. [55]
Age of those in adult drug treatment
For 2021/22, the largest proportions of clients accessing drug treatment in Surrey were aged between 30-39 (31%), 40-49 (29%) and 18-29 years (21%). This differs from the England average, where the highest proportions were in the 40-49 (34%), 30-39 (31%) and 50-59 (17%) age groups.
Age of those in adult alcohol treatment
In 2021/22, the largest proportions of adults accessing alcohol-only treatment were aged 40-49 (28%) followed by 50-59 years (27%), similar to the England average ages.
Age of those in young people’s drugs and alcohol treatment
The largest proportion of young people (aged up to 25 years) starting structured treatment within Surrey in 2021/22 were aged 16-17 years (40%), followed by those aged 18-24 (32%) and then 14-15 year olds (25%). Very few young people under the age of 14 were engaged in structured treatment in Surrey (4%).
The average England figures vary slightly, in that the 14-15 years (36%) and 16-17 years (35%) were the largest proportions, followed by the 18-24 year cohort (21%). This may be explained by the historic transitional arrangements between Surrey’s young people’s and adult services, where a clear pathway has been developed based on the young person’s needs and where they would be better suited.
Gender of those in adult drug treatment
70% of adults in drug treatment in Surrey in 2021/22 were men, similar to the England figure of 71%. The skew towards men is slightly higher for opiates (men = 71%) compared with non-opiates (men = 67%), which is similar to English figures. For adults starting drug treatment in 2021/22, 67% were men and 33% were women (for both opiates and non-opiates). This compares with the English figures of 74% men for opiates and 68% men for non-opiates.
Gender of those in adult alcohol treatment
The gender-split of adults in alcohol-only treatment in 2021/22 was similar in Surrey (57% male) and England (58% male).
Gender of those in young people’s drug and alcohol treatment
In 2021/22, 62% of young people in treatment were male and 38% were female, in both Surrey and England.
Smoking tobacco
Adults engaged with treatment in Surrey during 2021/22 who smoke tobacco was between 53% (alcohol) and 75% (opiates). This was higher than the national average of 45% to 67%. Referrals to smoking cessation services are available in treatment settings although there is no data available either at a local or national level for these referrals.
Deprivation
The majority of Surrey residents live in the most affluent areas in England. The majority (68.5%) of lower super output areas (LSOAs) in Surrey are in in the least deprived deciles 8, 9 and 10. There are no Surrey LSOAs in the most deprived decile 1, and just four (0.6% of areas) in the second most deprived decile 2, which are among the top five of Surrey’s 21 “key neighbourhoods” – neighbourhoods which experience the poorest health outcomes in Surrey [56]. These are parts of Westborough and Stoke wards (in Guildford), Hooley, Merstham and Netherne ward (Reigate & Banstead) and Canalside ward (Woking).
Deprivation of those in adult drug treatment
In 2021/22, a greater proportion of Surrey’s new presentations to adult drug treatment were in regular employment compared with England (36% vs 24%), and a lower proportion were unemployed (36% vs 48%). This could reflect Surrey’s relative affluence, compared with England as a whole. It could also indicate an underlying health inequality – for example, if those in regular employment in Surrey are more likely to be able to access drug treatment than those not in regular employment.
In 2021/22, the proportion of new presentations to adult drug treatment in Surrey who have no fixed abode (4%), or who have a housing problem (6%), was lower than the corresponding proportions in England (7% and 13% respectively). This could again reflect Surrey’s relative affluence, compared with England as a whole, or it could indicate a health inequality – for example, if drug users with housing problems in Surrey find it more difficult to access drug treatment than drug users without housing problems.
Deprivation of those in adult alcohol treatment
In 2021/22, a greater proportion of Surrey adults starting alcohol treatment were in regular employment compared with England (45% vs 37%), and a lower proportion were unemployed (35% vs 40%). This could reflect Surrey’s relative affluence, compared with England as a whole or indicate an inequality.
In 2021/22, the proportion of adults starting alcohol treatment in Surrey who have no fixed abode (1%), or who have a housing problem (2%), was lower than the corresponding proportions in England (2% and 7% respectively). This could again reflect Surrey’s relative affluence, compared with England as a whole or indicate an inequality.
Deprivation of young people in drug and alcohol treatment
The Crime Survey for England and Wales for 2020-2021 found that drug use among young people was more likely in low-income households. [57]
A higher proportion of people aged under 18 in treatment in Surrey were in mainstream education (71%) or employment (8%) at the start of their treatment compared with England (60% and 3% respectively). A lower proportion of young people in treatment in Surrey are not in education, employment or training compared with England at the start of their treatment (8% in England vs 12% in England).
A greater proportion of Surrey under-18s in treatment are living with their parents than the England equivalent (90% vs 82%). The proportion of Surrey under-18s living in unsettled accommodation or of no fixed abode is 0%. The proportion of English under-18s living in unsettled accommodation or of no fixed abode is 1% and 0% respectively.
Mental health
In Surrey in 2021/22, the estimated prevalence of common mental disorders for adults >16 years of age was 12.8% which was statistically significantly lower than 16.9% in England. [58]
For children and young people, in 2021/22, Surrey had higher rates than England for hospital admissions as a result of self-harm in 10-24 year olds, percentage of school pupils with social, emotional and mental health needs, and percentage of children looked after whose emotional wellbeing is a cause for concern. [59] The higher percentage of school pupils and children looked after with mental health needs or emotional concerns could relate to better recording of data in Surrey than in England, or could relate to truly higher rates of these conditions in Surrey.
Mental health of those in adult drug treatment
78% of Surrey females and 68% of Surrey males entering drug treatment in 2021/22 were identified as having a mental health need, compared with England’s rates of 81% and 66% respectively. This gender gap could reflect true differences in mental health needs by gender, or that women are more likely to report mental health needs/have their mental health needs identified by health services.
Of those adults in drug treatment identified as having a mental health treatment need, 84% of Surrey females and 77% of Surrey males were receiving treatment for their mental health, compared with 81% of English females and 72% of English males.
Mental health of those in adult alcohol treatment
73% of adults who entered alcohol only treatment in 2021/22 were identified as having a mental health treatment need compared to 70% in England. 84% of Surrey adults in alcohol only treatment identified as having a mental health treatment need were receiving treatment for their mental health, similar to 83% in England.
Mental health of those in young people’s drug and alcohol treatment
In 2021/22, 66% of Surrey females aged < 18 years old were identified as having a mental health need at the start of treatment, compared with 46% of males. This is higher than the corresponding proportions for England where 61% of females and 40% of males <18 years of age were identified as having a mental health need at the start of treatment. Of all young children in England aged 11-16 (including those not in treatment) included in the Mental Health of Children and Young People survey 2023, 22.3% of boys and 22.9% of girls have a probable mental health disorder. [60]
Possible explanations for Surrey having higher rates than England include true higher need locally, or better data recording in Surrey. This could particularly be the case given that Surrey has a designated Catch-22 mental health post integrated within CAHMS and therefore Surrey may be better at picking up young people than other areas in England.
Of those identified as having a mental health need, 90% of females and 70% of males were having that need met in Surrey, compared with 73% and 68% respectively in England. Reasons for the 20% gender disparity in mental health needs being met should be further explored.
Disability status of those in adult drug treatment
A higher proportion of adults in drug treatment in Surrey in 2021/22 had “no disability” (75%) compared with England (64%). It is important to ensure that people with a disability in Surrey who require drug treatment are not experiencing any barriers to accessing care.
Disability status of those in adult alcohol treatment
A higher proportion of adults in alcohol treatment in Surrey in 2021/22 had “no disability” (75%) compared with England (66%). It is important to ensure that people with a disability in Surrey who require treatment are not experiencing any barriers to accessing care.
Parental status of those in adult drug treatment
In 2021/22, there were more parents living with children and presenting to drug treatment in Surrey (26%) compared to England (15%). A lower proportion of Surrey parents in adult drug treatment do not live with their children compared with adults in England (3% in Surrey and 18% in England). In Surrey, there were more “Other contacts living with children” than England (7% vs 2%).
Parental status of those in adult alcohol treatment
In 2021/22, a higher proportion of new presentations to adult alcohol treatment services in Surrey than England were parents living with children (31% in Surrey vs 21% in England). A lower proportion are parents not living with children (2% in Surrey and 13% in England). A higher proportion are “other contact living with children” (6% in Surrey and 2% in England).
Parental status of those in young people’s drug and alcohol treatment
Surrey has a very low number (<5) of young people in drug and alcohol treatment who are parents living or not living with children. This proportion is lower than England’s rate, which is also low (<2%).
Outcomes for people in drug and alcohol treatment
Length of time in treatment for adults using drugs
Adults that have been in treatment for long periods of time (six years or over for adults with opiate problems and over two years for adults with non-opiate problems) will usually find it harder to successfully complete treatment. Current data shows that adults with opiate problems who successfully complete within two years of first starting treatment have a higher likelihood of achieving sustained recovery. [8]
In 2021/22, 38% of Surrey’s adults in treatment for opiate use were in treatment for less than two years, compared with 42% in England, and 26% were in treatment for six years or more, compared with England’s 28%.
For the same year, 2% of Surrey’s adults in treatment for non-opiate use were in treatment for over two years, compared with 3% of England’s adults.
Length of time in treatment for adults using alcohol
The length of a typical treatment period is just over 6 months, although nationally 12% of adults remained in treatment for at least a year. Retaining adults for their full course of treatment is important in order to increase the chances of recovery and reduce rates of early treatment drop out. Conversely, having a high proportion of adults in treatment for more than a year may indicate that they are not moving effectively through and out of the treatment system.
In 2021/22, Surrey’s average days in treatment was 130 days compared with England’s 194 days. In Surrey, 19% of exits from alcohol treatment were in treatment for <1 month compared with 8% in England. In Surrey, 30% of exits from treatment were in treatment for 1-3 months compared with 26% in England. Surrey and England had similar rates of people in treatment for 3-9 months. Surrey had fewer patients in treatment for 9-12 months than England (5% vs 8%) and for 1-2 years (5% vs 10%).
Length of time in treatment for young people using drugs and alcohol
Young people generally spend less time in specialist interventions than adults because their substance misuse is not as entrenched. However, those with complex care needs often require support for longer. For 2021/22, Surrey had a higher proportion of under 18s having treatment for 12 weeks or under than England, as a proportion of all exits from treatment (74% vs 40%), and a lower proportion of under 18s in treatment for longer (23% of Surrey under 18s were in treatment for 13-26 weeks, compared with 33% in England, and 4% were in treatment for 27-52 weeks compared with 19% in England, and none in Surrey were in treatment for over 52 weeks). This could be due to the service in Surrey referring onto appropriate services when required to avoid holding onto children and young people for longer than required. Although children and young people may be “closed” at the end of their treatment, Catch-22 continues to undertake welfare checks at regular intervals, which is not shown on NDTMS data.
In-treatment outcomes
Data from NDTMS suggests that adults who stop using illicit opiates in the first six months of treatment are almost five times more likely to complete successfully than those who continue to use substances. In 2021/22, Surrey’s rates of abstinence from drugs at six months review were 55% for opiates compared with England’s 45%; 53% for crack cocaine compared with 39% for England; 41% for cannabis compared with England’s 38%; 14% for amphetamines compared with England’s 57% (but numbers were very small – < 5 – so it is not possible to determine if this was statistically significant), and 33% for adjunctive alcohol use compared with England’s 29%.
Surrey’s rate of adults no longer injecting at six months review was 79% vs England’s 59%.
Successful completions for drug treatment
In 2021/22, the proportion of people in treatment for non-opiates (including alcohol), who successfully completed treatment and did not re-present within 6 months was higher in Surrey (42%) than in England (34.3%), and for opiates was 6% in Surrey and 5% in England.
In 2021/22, compared to the previous year, successful completion rates for alcohol and non-opiate treatment decreased by 11 percentage points in Surrey, whereas in England successful completion rates increased by 11.4 percentage points.
The rate of successful completions for opiate treatment has declined since 2010 in Surrey and England, as per the figure below.
Figure 8: Successful completion of drug treatment: opiate users [62]
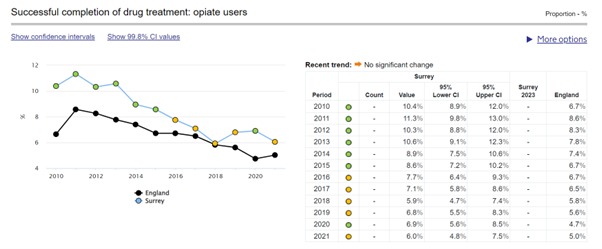
Successful completions for alcohol treatment
For 2021/22, Surrey had a higher rate (73%) of people leaving alcohol treatment compared to England (63%). However, Surrey had only a slightly higher rate (39%) of successful completions for alcohol treatment compared to England (37%). Therefore, overall, Surrey had a lower proportion of adults successfully leaving alcohol treatment (53%) compared with England (59%).
Compared to the previous year, successful completion rates for alcohol and non-opiate treatment in 2021/22 decreased by 11 percentage points, whereas in England successful completion rates increased by 11.4 percentage points.
For 2021/22, a lower proportion of adults in treatment for alcohol use became abstinent compared with England (45% vs 50%).
Stakeholder insights
Engagement was undertaken with key groups and services including mental health, Hepatitis Operational Delivery Network, GP forums, housing and education leads from local authorities, substance misuse treatment providers for adults and children & young people, and the Police. Discussion focussed on gaps and obstacles, and opportunities and solutions. Draft findings from the JSNA were also shared with the Combatting Drug Partnership members. It is noted that stakeholder feedback included here focuses mainly on areas for improvement. Below is a summary of themes and issues that were highlighted:
Prevention: stakeholders highlighted the importance of prevention and strengthening training and support to non-specialist services, including teachers, social workers and police. Multi-agency training on substance misuse and related harms and links with related issues such as mental health, self-harm and sexual health was proposed. Targeted prevention support for children looked after, care leavers and young carers was identified as an opportunity. Developing a collaborative approach to preventing the increase in use and normalisation of cannabis was highlighted by several stakeholder groups, including opportunities to provide information/myth-busting to non-specialist workforce regarding effects of cannabis.
Person-Centred approaches: this was a priority for many stakeholders, including concerns about the need for more outreach/support workers to help people navigate the system, avoid non-engagement, attend appointments, maintain housing placements. Getting to appointments can be expensive and difficult on public transport and inconsistent contact details resulting in difficulties registering with a GP, were also highlighted. This was especially important for people with chaotic behaviours in the community and rough sleepers. The needs of people with multiple disadvantage, including problematic substance use, mental health issues and neurodiversity were highlighted and the need for trauma-informed care training for all staff was proposed. Concerns about a lack of Fellowship groups were raised. Challenges included focusing on needs-based rather than diagnosis-based approach to service design, which builds in flexibility. Opportunities to strengthen person-centred approaches included embedding peer mentors in aftercare and recovery support, recognising that workers with lived experience have an important role and can help people believe that change is possible. Strengthening service user involvement and co-production throughout pathways was highlighted. The opportunity to develop a hybrid online and in-person recovery support model was proposed.
Substance use services: stakeholders identified a range of concerns including: inconsistent investment in alcohol liaison teams in acute settings, access to residential detoxification not being available within the County due to the unit for Surrey being closed down due to funding constraints, concerns about long waits for social care assessments, need for more out of hours services, increased awareness about one-stop shop drop ins/warm spaces, need for more cannabis-specific interventions. It was suggested that crisis cards including helpline and out of hours services should be widely available. Concerns about fragmentation of funding for blood-borne virus testing and short-term funding for networks were highlighted, but opportunities included strengthening interfaces with probation services around blood-borne screening and liver health checks.
Mental health: Mental health issues were raised by many stakeholders. This included concerns about people falling through the gap between mental health and substance use services, and people, including young people, being told they must engage with substance use services before they can access mental health services. It was reported that the most complex patients are also the most likely to be affected by exclusion criteria when accessing services. There were also concerns about a rising number of Section 42 mental health referrals having a negative impact on social care assessments. However, stakeholders thought there was an opportunity to work across the system/services to better understand the challenges and how best to support people and a deep-dive into substance misuse-mental health pathways was proposed and the development of more in-reach mental health services to provide support when people may be more receptive to addressing substance misuse issues.
Criminal Justice: Opportunities identified by stakeholders included ensuring drug testing on arrest, which is being developed, includes pathways into appropriate support and treatment services; exploring wider roll out and availability of Naloxone through the criminal justice system, including the Police; the need to ensure there is capacity in the system for education and treatment if numbers are increased through proposed introduction of tougher consequences for possession; increased use of bail conditions and other measures such as Drug Rehabilitation and Alcohol Treatment Requirements; the need to develop more information sharing between agencies on discharge, including prisons.
Recovery: A range of gaps were identified by stakeholders including: more support needed for people leaving residential rehabilitation and housing pathways to meet the needs of high-needs clients and appropriate placements so that tenancies do not fail, which is a concern especially in the private rented sector; more supported living placements, other than abstinence/dry houses; concerns about people placed in emergency accommodation out of County which makes it difficult to access support/treatment. However, several opportunities were identified including: a new wellbeing and prevention pathway for residential rehabilitation; a dedicated senior social care assistant benefits and housing practitioner and access to General Practice Integrated Mental Health Services supporting independence and access to mental health rehabilitation teams. The need for more partnership with the Department of Work and Pensions to improve employment opportunities was identified.
Collaboration: many stakeholders identified the need for more pro-active partnership working across services and the need to address the challenges of information sharing between agencies was identified. Examples of collaboration included use of shared joint clinic space in community hubs and use of joint local quality assurance guidelines. Lots of opportunities for strengthening collaboration were identified including: a revised standard operating procedure on collaborative working between providers; more information sharing across providers, including briefing to better understand processes and access to support; workforce development, joint training and education using the evidence base of what is effective with wider workforce and developing skills around associated risks and vulnerabilities including exploitation and county lines and safeguarding and referrals of vulnerable adults under the Care Act (2014); developing a shared communications plan that includes sharing stories of recovery.
The opportunity to collaborate on addressing the normalisation of cannabis was identified by several stakeholder groups and the development of a multi-agency problem solving approach to tackling increasing cannabis use was proposed. Other areas where collaborative work is underway includes strengthened links between children and young people’s substance misuse services and community Police, and children’s homes, as well as link workers in mental health, the child exploitation and missing unit, probation and youth offending services and with children’s homes.
Workforce: a number of workforce challenges were identified including need for greater resources to develop the workforce, and challenges of recruitment, especially of professionally registered, experienced staff within substance misuse services; multi-agency workforce development was a theme throughout the engagement and has been included across this summary. Concerns were also expressed about staff changes and a loss of organisational memory and understanding at a leadership level.
Feedback from service users and others affected by drug related harm
The CDP has commissioned a public involvement service (Luminus, also home to Healthwatch Surrey) to engage with people with lived experience and their families and friends and others affected by drugs and/or alcohol in a new, two-year process. Luminus synthesises these insights into reports which are shared with the CDP and inform the CDP delivery plan. Findings from the first two quarterly reports and a public engagement event are included below from carers, service users, and frontline staff. There are six quarters of reports still to come.
The below findings should be interpreted in the context of public engagement reports:
- Which represent specific snapshots in time.
- People are more likely to report things they feel could be improved with services, rather than comment on things they feel are going well.
- The views of individuals reflect their personal experiences and perceptions, and are important in providing insights.
Insights into the public’s experience is likely to evolve as further quarters’ reports are collated.
This feedback relates to all services, which may include substance misuse, adult social care, mental health care, the criminal justice system, housing, and primary care.
Below is a summary of themes and issues that were highlighted:
Barriers to access
Some people who misuse substances reported:
- Stigma and self-stigma, including perception of the system or an individual worker stigmatising them.
- Treatment provided in buildings that are almost too local.
- Lack of awareness that self-referral is possible to access treatment and recovery services, or experiencing barriers to access.
- Not getting replies to contacting services by email or telephone.
- Not feeling listened to when raising concerns to services.
- One perception was fed back that some people who use support services e.g. Hope Hub, Renewed Hope, may agree to be referred to substance misuse services, but this may be more a tick box exercise, as stopping the one thing that makes their life bearable (drugs or alcohol) isn’t a priority – finding accommodation and a warm meal is.
- Rigid processes that don’t work for all.
Communication and signposting
- GPs and other frontline health staff may not be aware of all services, or may not signpost to services.
- Some service users had experienced the helpfulness of being signposted and becoming involved in Alcoholics Anonymous, Cocaine Anonymous and Narcotics Anonymous.
Mental health and substance misuse
Some service users reported:
- A perception of a lack of appropriate support for the underlying trauma that caused them to start misusing substances.
- Not wanting to stop using substances as it helps them to cope with their mental health, which may not be being treated.
- A perception of not being able to access mental health treatments while using substances.
- Not knowing what services are available to them, e.g. mental health services.
- Feeling they would benefit from different treatments than the options they are offered e.g.
- preferring trauma counselling over cognitive behavioural therapy sessions
- preferring to be offered counselling rather than just medication
- preferring one-to-one and face-to-face counselling rather than group therapy or online therapy (or vice versa)
- insufficient number of treatment appointments, including counselling appointments
Continuity of care and establishing trust
Some service users fed back:
- Seeing a different GP or consultant each time makes it harder due to having to start from scratch each time with their complex history, and can be triggering particularly if patients have a history of trauma.
- Lack of knowledge of who can help with complex issues e.g. dental concerns, housing concerns.
- Lack of follow up from services.
- The usefulness of mentors, e.g. probation officers, with lived experience who can relate to their audience can help people get out of gangs/drugs.
- The helpfulness of living in shared accommodation with other people trying to support each other.
The latest Luminus report also included positive feedback, including that one service user reported having cut down their alcohol intake because of an i-access worker really helping them; another service user said the person at i-access was great and had lived experience which helped reassure them; one person reported that Catch-22 helped them so much that they have been sober for five years; another interviewee reported that their relative used i-access and found them “really good”.
Carers
Some carers reported:
- Feelings of guilt and anxiety that their loved one is suffering from addiction.
- Difficulties getting their loved one to engage with services, particularly if they have other conditions e.g. neurodiversity/personality disorders, and associated social issues e.g. rape and self-harm.
- Some people who misuse substances need consistent help and encouragement to engage with care, but some carers feel that help is not there.
- Caring for a person dependent on drugs is an isolating experience due to stigma and lack of experience, knowledge and skills in dealing with addiction, meaning lack of the usual support network of family and friends.
- A perception of lack of rehabilitation options resulting in carers paying themselves which they may not be able to afford.
- Perception of lack of available support for carers of people with dependent substance misuse.
- Carers’ and families’ lives go on hold while trying to deal with the addiction.
- Concerns about long waiting lists for counselling.
- Single, accessible point of care from i-access provided one carer with
- valuable continuity of care
- signposted carer to counselling services
- provided advice on how to register as a carer and subsequent available financial support for carers
- reduced stress, fear and loneliness and increased strength and confidence
Service user feedback
I-access collects feedback from i-access and VIA service users regularly and reviews this on a regular basis. Feedback from service users is taken into account and included in the “You said, we did” section of the patient experience report which is published regularly and shared with the SABP mental health and substance use program board.
Work taking place to improve the system in Surrey
There is a wide range of activity already taking place across Surrey which represents some of the collaborative work taking place in the county.
Supporting people into treatment
Research is being undertaken to look at how to better engage with people who misuse substances and improve self-referrals into the system.
Improvements to joint working between mental health and substance misuse services are underway, including members of both services attending “no bounce workshops”, a mental health improvement action plan from SABP NHS trust including appointment of new staff members to improve joint working, and the community mental health service SOPs being rewritten. i-access have a specialist co-occurring conditions worker now in post, and Care Pathway Forums are now in place.
Treatment journey
Work is underway to understand Surrey’s relatively high rate of adults leaving substance misuse treatment in an unplanned way. There could be many possible explanations for this, including relating to data recording (for example, if Surrey records early exits more accurately than other parts of England) or patients feeling their needs are unmet by services. This is a key performance indicator for the service and is being reviewed regularly and there are plans to expand outreach provision in future to reengage those who drop out of treatment.
There is ongoing development of referral and engagement processes between the Criminal Justice System and community treatment. The plan includes testing on arrest, video assessments between prisons and community keyworkers, and a community treatment team prioritising those engaged with probation.
Funding has been identified by SCC Public Health for placements in residential rehabilitation for people who do not meet the criteria for adult social care funding.
Wider services
The impact of the closure of pharmacies on service users is being monitored by Surrey County Council, i-access, and the Local Pharmaceutical Committee.
Surrey County Council will be implementing the “Swap to Stop” smoking cessation initiative within treatment services from 2024.
Reducing deaths from drug misuse
As a result of Surrey’s 2021 drug-related death audit, Surrey County Council are commissioning a new database to collate information gathered from suicides and drug related deaths. Real-time surveillance will allow timely learning and appropriate responses, rather than waiting for Coroner’s inquests to be completed.
Surrey County Council has also launched an online tool for the reporting of non-fatal overdoses by individuals and professionals, in order that more understanding of overdoses can be gathered and that resources can be put in place to minimise risk.
Surrey County Council also commissions a telephone/online counselling service for those affected by a drug-related death or non-fatal overdose. The service also provides virtual counsellor-facilitated groups for those who have completed their counselling programme.
Strengthening recovery – wider determinants
Surrey County Council have recently commissioned a support service for carers of people with mental health needs and/or substance misuse needs, inclusive of parent carers and young carers.
It is a small pilot service that links with the Surrey universal carer hub offer.
Individual placement and support (IPS) is a DWP-funded individual placement and support service which is currently being set up in Surrey and due to start next year, to help provide employment support to people who misuse substances.
Information sharing and intelligence.
Luminus (also home to Healthwatch Surrey) is engaging quarterly with people impacted by drug and alcohol use and feeding back their findings to the CDP.
The CDP launched a web page to allow information sharing with the public about the work the CDP is doing locally. Surrey Combating Drugs Partnership | Healthy Surrey
The CDP are appointing a data and digital lead.
Work taking place to improve the system in Surrey – young people
There are a number of interventions in place to support the offer to young people within Surrey:
SCC has commissioned a service to update the schools’ guidance for drugs, alcohol and smoking education. The guidance is supported by partners and will be launched in September 2024. It will be available to all Surrey schools.
SCC has commissioned the development and delivery of drug, alcohol and tobacco toolkits for all key stages. The toolkits will give accurate and age-appropriate information and lesson plans to help support teaching staff to deliver information in relation to drugs, alcohol and tobacco. The toolkits will be available from September 2024.
SCC continues to invest funding in the development of substance use posts across the system, including integrating Catch 22 workers within youth justice, child exploitation/missing, mental health and probation teams. In addition, Catch 22 are developing new posts to help support the education system in reducing the number of drug-related exclusions, which are higher in Surrey than nationally.
SCC endorses the Family Safeguarding Model to support families impacted by parental substance use. A designated team within iaccess works with parents in treatment where child protection concerns have been flagged. The iaccess workers work closely with colleagues in children’s social care to ensure the social needs of the child and family are met.
There is also a designated psychology team from SABP, based in SCC teams, that support the parents where child protection concerns have been raised. They offer motivational counselling and CBT to the parents.
Surrey County Council have recently commissioned a support service for carers of people with mental health needs and/or substance misuse needs, inclusive of parent carers and young carers.
It is a small pilot service that links with the Surrey universal carer hub offer.
Recommendations
These recommendations include a rationale and have been mapped against the four Subgroups for the Combating Drugs Partnership:
SG 1. Breaking drug supply chains
SG 2. World class treatment and recovery system
SG 3. Achieving a generational shift in demand for drugs
SG 4. Reducing alcohol and tobacco related harm
Prevention and Early Intervention
| Recommendation | SG1 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Ensure ongoing high profile universal and targeted campaigns on reducing alcohol consumption among adults and young people.
Rationale: A higher proportion of Surrey adults drink >14 units alcohol per week, compared with England. There has been an increase in alcohol-related hospital admissions in Surrey over the past decade, and an increase in numbers in treatment for alcohol dependence. Prevention and early intervention initiatives can support individuals to make informed decisions and prevent longer-term drug and/or alcohol use and engagement in associated risky behaviours. |
n/a | n/a | Yes | Yes |
| Embed and strengthen education for professionals and young people on substance use in school, and out of school, settings, including addressing normalisation of cannabis.
Rationale: A higher proportion of Surrey young people in treatment reported problems with alcohol, compared with England. In the 28 days prior to starting treatment for substances, under-18s in Surrey had a higher proportion of heavier drinkers than under-18s in England. Prevention and early intervention initiatives can support individuals to make informed decisions and prevent longer-term drug and/or alcohol use and engagement in associated risky behaviours. Cannabis use in young people was highlighted in stakeholder feedback. |
n/a | n/a | Yes | n/a |
| Strengthen pathways between health, social services and drug services to identify and intervene early with vulnerable children and families.
Rationale: Nationally, 3% of young people in community structured substance misuse treatment are children looked after compared with 1% in Surrey (n=8). However, this apparent difference may be misleading due to reporting differences. In the stakeholder feedback, many stakeholders identified the need for more pro-active partnership working across services and the need to address the challenges of information sharing between agencies was identified. |
n/a | n/a | Yes | n/a |
Supporting people into treatment
| Recommendation | SG1 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Tackle stigma related to substance use, to enable more people to seek treatment and build supportive communities. Encourage CDP partners to undertake stigma training.
Rationale: Surrey people with lived experience and their carers reported perceived stigma as a barrier to accessing care. Stigma and unconscious bias may influence service providers across the system and result in a lower standard of care and housing for people who misuse substances. Bringing treatment and recovery services for drug dependence up to parity with other health, care and housing services will require improvements in coordination and accountability. |
Yes | Yes | Yes | Yes |
| Explore the reasons for Surrey’s higher than England reported rates of unmet need in opiates and crack -cocaine.
Rationale: Surrey has higher estimated rates of unmet need for people who use opiates and crack-cocaine compared with England. Understanding the reasons for this could help us address any potentially identified causes and as a result better meet the needs of people who misuse substances. |
n/a | Yes | n/a | n/a |
| Continue to strengthen pathways between mental health and substance use services to ensure that people are able to access the right care where there is a dual diagnosis.
Rationale: Stakeholder feedback from multiple stakeholders including GPs, mental health services, and Luminus all indicated that complex patients with both mental health and substance misuse needs are the most likely to be affected by exclusion criteria when accessing services. |
n/a | Yes | n/a | Yes |
| Continue to review work by Solutions Research and CDP partners to optimise communication and referral pathways into substance misuse services in Surrey.
Rationale: A lower proportion of adults in treatment in Surrey than nationally were self-referrals or through the criminal justice system, and a higher proportion from health or social care. Service users and carers in Surrey reported to Luminus that they did not know where to look for help, and quite a lot of “digging” was required to find the correct self-referral pathways. Carers reported they might have given up trying to find help if they had needed to get help for themselves. The ambition is to ensure Surrey residents feel confident in accessing information and engaging proactively with treatment services, ensuring that people receive the support they need when they need it. |
Yes | Yes | Yes | Yes |
| CDP to investigate where there are discrepancies in CJIT data recording to ensure accurate data reporting.
Rationale: There are discrepancies between Surrey probation data and NDTMS data. Having an accurate understanding of referral pathways will allow accurate interventions to be undertaken to improve referral processes. |
Yes | Yes | n/a | n/a |
| Increase engagement by Surrey prison leavers in community drug and alcohol treatment, increasing referrals from the criminal justice system including prisons and probation service. This includes reviewing the needs of male remand prisoners from Surrey in HMP Wandsworth (the main male remand prison for Surrey residents) to ensure effective pathways into treatment and recovery support.
Rationale: Compared with England, a lower proportion of people in treatment in Surrey were referred in by the criminal justice system; a lower proportion of CJS referrals were from prisons; and a lower proportion of CJIT adults were in contact with the treatment system. Compared with England, Surrey prison-leavers had lower rates of engagement with treatment after leaving prison, however this may be due to data-recording error which is currently being addressed by the prisons and treatment service. |
Yes | Yes | n/a | n/a |
| Optimise the introduction of Police custody ‘test on arrest’ and subsequent referral into treatment.
Rationale: Compared with England, a lower proportion of CJS referrals were arrest referrals. The Harm to Hope strategy aims to engage new presentations in treatment and reduce ongoing drug-related crime. |
Yes | n/a | n/a | n/a |
| Optimise the use of drug rehabilitation and alcohol recovery requirements/programmes within the criminal justice system.
Rationale: Compared with England, a lower proportion of CJS referrals were ATRs and DRRs. There has been a reduction in the use of DRRs and ATRs nationally over time and it is recognised that offering these community sentences will reduce reoffending. |
Yes | Yes | n/a | n/a |
| Understand and optimise referrals for young people from education settings and youth criminal justice settings.
Rationale: Compared with England, a lower proportion of young people in treatment were referred from education settings and youth criminal justice settings. The ambition is that all residents can access treatment at the most relevant time whilst motivated wanting to engage in treatment. |
Yes | n/a | Yes | n/a |
Treatment journey
| Recommendation | SG2 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Continue to explore reasons for, and reduce the rate of, people leaving treatment in an unplanned way before 12 weeks. Understand why more men than women leave treatment early in an unplanned way, including reviewing access to support.
Rationale: A higher proportion of people in treatment for substance misuse in Surrey than England leave treatment in an unplanned way before 12 weeks. A higher proportion of men than women leave treatment in an unplanned way in Surrey. |
n/a | Yes | n/a | n/a |
| Work to understand treatment progress, including why Surrey appears to have a lower rate of successful completions for opiate treatment in adults compared with England.
Rationale: Compared with England, Surrey has a lower rate of successful completions for opiate treatment among adults. |
n/a | Yes | n/a | n/a |
| Work to understand and increase successful completions for alcohol treatment among adults.
Rationale: Compared with England, Surrey has a lower rate of successful completions for alcohol treatment among adults. |
n/a | Yes | n/a | n/a |
People experiencing multiple disadvantage
| Recommendation | SG1 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Continue to coproduce and improve engagement with people who experience multiple disadvantage and develop trauma informed practice, including learning from the Changing Futures programme and Multiple Disadvantage JSNA chapter.
Rationale: Feedback from stakeholders, people with lived experience, and their carers is that people who misuse substances have often experienced trauma, and some of the ways the current health and care system functions either do not take this into account, or can exacerbate it, for example by resulting in people having to retell their story and resulting in re-traumatisation. |
Yes | Yes | Yes | Yes |
| Improve understanding of the Care Act 2014 among organisations who work with vulnerable people such as people with multiple disadvantage, and improve understanding of the importance of referring to adult social care for assessment at the earliest opportunity rather than waiting until the person is in crisis.
Rationale: stakeholder feedback particularly from adult social care indicates that there may be a lack of awareness among professionals of the importance of referring to adult social care early for assessment |
Yes | Yes | Yes | Yes |
Wider services
| Recommendation | SG1 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Continue to monitor the impact of pharmacy closures on harm reduction measures for service users.
Rationale: stakeholder feedback indicates that pharmacy closures may reduce the accessibility of harm reduction measures such as opiate substitute therapy and sterile injecting equipment, resulting in increased harm to people who misuse substances. |
n/a | Yes | n/a | n/a |
| Review the smoking cessation offer to people who use substances as part of new smoking cessation contract with new provider.
Rationale: A higher proportion of adults in treatment for substance misuse in Surrey than England smoke at initial assessment, and a lower proportion are abstinent from smoking at 6-month review. Smoking is a high-risk factor associated with drug-related deaths, and so providing a smoking cessation offer in treatment services will reduce the risk of drug-related death. |
n/a | n/a | n/a | Yes |
Inequalities
| Recommendation | SG1 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Better understand the interactions between protected characteristics and substance misuse in Surrey. Undertake a review to understand unmet need in Surrey, including if ethnic, gender, deprivation and disability differences of those in drug treatment in Surrey represent unmet need/barriers to access. Rationale: There are differences in proportion of people from certain demographic groups, including certain protected characteristics, accessing treatment in Surrey. Understanding the reasons for these differences would allow us to identify any barriers to accessing services experienced by these groups, and allow us to address these. Understand and address the higher rate of alcohol-related liver and/or cardiovascular disease in Runnymede, Spelthorne, Woking and Guildford than England. Rationale: Runnymede and Spelthorne are both above the national average in terms of alcohol-related liver and cardiovascular disease, Guildford is above the national average in cardiovascular disease and Woking is above the national average in alcohol-related liver disease. |
Yes | Yes | Yes | Yes |
Reducing deaths from drug misuse
| Recommendation | SG1 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Continue to increase awareness and availability of naloxone within the community.
Rationale: A lower proportion of eligible Surrey adults in opiate treatment were issued with naloxone than adults in England. The use of naloxone is important in reducing opioid-related deaths and is accessible to everyone through participating pharmacists and community services. |
n/a | Yes | n/a | n/a |
| Develop a partnership response to drug related deaths through a DARD (drug and alcohol-related deaths review system) approach.
Rationale: In 2021 an audit of drug related deaths identified a range of complex characteristics of individuals who died; a partnership response to understanding drug-related deaths is important in order to identify themes and respond accordingly. |
n/a | Yes | Yes | n/a |
| Undertake a 3-yearly drug-related death audit in partnership with Surrey Coroners’ Office.
Rationale: The last audit was undertaken in 2021. A new audit of completed coroner’s drug-related death inquests will provide updated themes and inform service development and commissioning. |
n/a | Yes | Yes | n/a |
| Build our intelligence of drug related deaths and overdoses, including promoting the use of the non-fatal overdose online reporting tool and implementing real-time surveillance of suspected drug-related deaths.
Rationale: More timely intelligence on the causes and themes of both overdoses and drug related deaths will support the reduction of drug-related deaths by providing learning for partners and inform changes to services as appropriate. |
Yes | Yes | Yes | n/a |
Strengthening recovery – wider determinants
| Recommendation | SG1 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Review the appropriateness of housing options for people who misuse substances, including people with alcohol-related brain injury. JSNA Housing and Related Support | Surrey-i (surreyi.gov.uk)
Rationale: Stakeholder feedback indicated that access to appropriate housing is an issue in Surrey. People who misuse substances need a holistic approach to their treatment in order to have the best chance of recovery. |
n/a | Yes | n/a | n/a |
| Improve access to accommodation within Surrey alongside treatment for homeless population, especially rough sleepers, to maintain continuity of care.
Rationale: Stakeholder feedback indicated that access to appropriate housing is an issue in Surrey. People who misuse substances need a holistic approach to their treatment in order to have the best chance of recovery. |
n/a | Yes | n/a | n/a |
| Improve employment opportunities, linking employment support and peer support to Job-Centre Plus services, and deliver the roll-out of Individual Placement Support (IPS) from 2024.
Rationale: although our employment rate for people starting treatment is higher than national it is still lower than the general employment rate for 16-64 year olds in Surrey. |
n/a | Yes | n/a | n/a |
| Optimise support for adult carers and young carers of people who misuse substances.
Rationale: stakeholder feedback indicated that there is a perception of lack of support for carers. |
n/a | Yes | n/a | n/a |
Information sharing and intelligence
| Recommendation | SG1 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Improve data sharing among partners to understand longer term outcomes of treatment and recovery.
Rationale: Understanding longer term outcomes in Surrey may help us identify areas that should be targeted for improvement. |
Yes | Yes | Yes | Yes |
| Develop local outcomes framework to ensure on-going monitoring and review.
Rationale: Sharing data across public health, criminal justice, and other CDP partners is complex, particularly as this is the first year it has been done in this way, and a local framework would help make it easier for everyone to know what data is expected of them, and help develop processes to share this data. |
Yes | Yes | Yes | Yes |
| Improve data exchange from ambulance provider via SODA to ensure adequate monitoring of and understanding of naloxone treatment use in the community.
Rationale: Surrey’s rate of people in treatment being offered naloxone is lower than England’s. In Surrey’s drug related deaths audit, naloxone was only used in 4 of the 91 deaths where opiates were present. |
n/a | Yes | n/a | n/a |
OHID data recommendations
| Recommendation | SG1 | SG2 | SG3 | SG4 |
|---|---|---|---|---|
| Include comparison with Chartered Institute of Public Finance and Accountancy (CIPFA) nearest neighbours in commissioning support pack to allow regional comparisons to be drawn.
Rationale: Surrey is a two-tier authority and therefore comparison with similar authorities with similar challenges that tend to be shared by two-tier authorities rather than unitary authorities would allow for a more accurate measure of its performance and help identify areas for improvement. |
n/a | n/a | n/a | n/a |
| Include quality outcomes in addition to process outcomes, which would help understand and evaluate local services.
Rationale: The OHID commissioning support pack at present has no measures of quality outcomes, only process outcomes; measuring quality outcomes would help identify ways in which Surrey services could improve their offer. |
n/a | n/a | n/a | n/a |
| Include successful completions and non-representations at 12 and 18 months in addition to the current 6 months. This would give a more nuanced understanding of the patient journey and where to target improvements.
Rationale: Substance misuse is a chronic, relapsing and remitting condition, where re-presentation to treatment may be an important part of someone’s treatment journey. Some people may present at longer intervals than six months, and these people are not being picked up by the current data recording mechanisms in the commissioning support packs. Understanding people’s treatment journeys may help Surrey services to make improvements. |
n/a | n/a | n/a | n/a |
Key Combating Drugs Partnership contacts
Lead contributors
| Amreet Battu | Public Health Registrar, Surrey County Council |
| Martyn Munro martyn.munro@surreycc.gov.uk |
Senior Public Health Lead, Surrey County Council |
| Heather Ryder Heather.ryder@surreycc.gov.uk |
Senior Public Health Lead, Surrey County Council |
| Kanchan Bhanage kanchan.bhanage@surreycc.gov.uk |
Combating Drugs Partnership Coordinator, Surrey County Council |
| Yazmin Castillo-Hodgson yazmin.castillohodgson@surreycc.gov.uk |
Alcohol Lead, Surrey County Council |
| Marcus Butlin marcus.butlin@surreycc.gov.uk |
Public Health Information Analyst, Treatment Data Lead, Surrey County Council |
| Sarah Crosbie sarah.crosbie@surrey.pnn.police.uk |
County Lines Coordination Manager Surrey Police |
| Russell Styles | Consultant in Public Health, Surrey County Council |
| Julia Groom julia.groom@surreycc.gov.uk |
Consultant in Public Health, Surrey County Council |
Acknowledgements
We would like to acknowledge the help and support of Lisa Sian (Luminus), Sally Reader (Probation Services), Mark Bamford (Probation Services), Camilla Bertoncin (Surrey County Council).
Bibliography
[1] “World Health Organisation. (2015). Management of Substance Misuse,” [Online].
[2] “ONS deaths related to drug poisoning,” [Online]. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsrelatedtodrugpoisoninginenglandandwales/previousReleases
[3] “Dame Carol Black report: summary of key findings,” [Online]. Available: https://www.gov.uk/government/publications/review-of-drugs-phase-one-report/review-of-drugs-summary#summary-of-key-findings
[4] “Preparing for a future threat,” [Online]. Available: https://www.gov.uk/government/publications/fentanyl-preparing-for-a-future-threat/guidance-for-local-areas-on-planning-to-deal-with-fentanyl-or-another-potent-opioid
[5] NICE, “NICE clinical knowledge summary: alcohol problem drinking,” [Online]. Available: https://cks.nice.org.uk/topics/alcohol-problem-drinking/background-information/definition/
[6] “Alcohol: Applying All Our Health,” [Online]. Available: https://www.gov.uk/government/publications/alcohol-applying-all-our-health/alcohol-applying-all-our-health
[7] “Health survey for England: Alcohol,” [Online]. Available: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2021/part-3-drinking-alcohol
[8] “Adult Drug Commissioning Support Pack and the Treatment and recovery unmet need toolkit” [Online] NDTMS – Home
[9] “Adults alcohol commissioning support pack” [Online] NDTMS – Home
[10] “Young people commissioning support pack” [Online] NDTMS – Home
[11] “Combating Drugs Outcomes Framework: Supporting metrics and technical guidance,” [Online]. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1158290/National_Combating_Drugs_Outcomes_Framework_-_Supporting_metrics_and_technical_guidance_PDF__1_.pdf
[12] “Independent review of drugs by Dame Carol Black,” [Online]. Available: https://www.gov.uk/government/collections/independent-review-of-drugs-by-professor-dame-carol-black
[13] “From harm to hope,” [Online]. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1079147/From_harm_to_hope_PDF.pdf
[14] “Guidance for local delivery partners,” [Online]. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1092762/Guidance_for_local_delivery_partners_July_2022.pdf
[15] “ONS crime and justice articles,” [Online]. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/drugmisuseinenglandandwales/yearendingjune2022
[16] “NHS Digital smoking, drinking and drug use in young people,” [Online]. Available: https://digital.nhs.uk/data-and-information/publications/statistical/smoking-drinking-and-drug-use-among-young-people-in-england/2021/data-tables
[17] “OHID local alcohol profiles for England,” [Online]. Available: https://www.gov.uk/government/statistics/local-alcohol-profiles-for-england-lape-march-2023-update/local-alcohol-profiles-for-england-short-statistical-commentary-march-2023
[18] “Surrey Substance Misuse JSNA 2017,” [Online]. Contact jsnafeedback@surreycc.gov.uk for this content.
[19] “Drug misuse prevention review,” [Online]. Available: https://www.gov.uk/government/publications/drug-misuse-prevention-review/acmd-drug-misuse-prevention-review-accessible
[20] “Health Matters,” [Online]. Available: https://www.gov.uk/government/publications/health-matters-harmful-drinking-and-alcohol-dependence/health-matters-harmful-drinking-and-alcohol-dependence#:~:text=National%20Institute%20for%20Health%20and,illness%20such%20as%20acute%20pancreatitis
[21] “Multiple needs and exclusions,” [Online]. Available: http://meam.org.uk/multiple-needs-and-exclusions/
[22] “Statutory homelessness in England: financial year 2021-22,” [Online]. Available: https://www.gov.uk/government/statistics/statutory-homelessness-in-england-financial-year-2021-22
[23] “Prevalence and unmet need toolkit,” [Online]. Available: https://www.ndtms.net/NDTMSReports/PrevalenceAndUnmetNeedToolkit
[24] “UKHSA survey of HIV and viral hepatitis among PWID,” [Online]. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1097419/UKHSA-UAM-survey-of-HIV-and-viral-hepatitis-among-PWID-2022-report.pdf
[25] [Online]. Available: https://www.surreyi.gov.uk/census-2021/ethnic-group/
[26] “Characteristics of children in need, Reporting year 2022,” [Online]. Available: Children in need, Reporting year 2022 – Explore education statistics – GOV.UK (explore-education-statistics.service.gov.uk)
[27] “Education statistics – permanent and fixed period exclusions,” [Online]. Available: https://explore-education-statistics.service.gov.uk/find-statistics/permanent-and-fixed-period-exclusions-in-england
[28] “Fingertips: Deaths from drug misuse, trends 2001-2018,” [Online]. Available: https://fingertips.phe.org.uk/search/drug#page/4/gid/1/pat/15/ati/502/are/E10000030/iid/92432/age/1/sex/4/cat/-1/ctp/-1/yrr/3/cid/4/tbm/1
[29] “Dame Carol Black Executive Summary Phase One February 2020,” [Online]. Available: https://assets.publishing.service.gov.uk/media/5f02e08ce90e075c5128f311/2SummaryPhaseOne+foreword200219.pdf
[30] “Review of drugs evidence pack,” [Online]. Available: https://assets.publishing.service.gov.uk/media/5eafffedd3bf7f65363e4fda/Review_of_Drugs_Evidence_Pack.pdf
[31] “Proven reoffending gov.uk statistics,” [Online]. Available: https://www.gov.uk/government/statistics/proven-reoffending-statistics-october-to-december-2021
[32] S. Police, Drugs Market Profile – Surrey Market, June 2023
[33] “National Crime and Policing Measures Report,” 2022. [Online]. Available: https://www.surrey-pcc.gov.uk/wp-content/uploads/2022/11/Performance-report_National-Policing-Priorities_Sept-2022.pdf
[34] “Monthly hospital admissions for assault by sharp object,” [Online]. Available: https://digital.nhs.uk/supplementary-information/2022/monthly-hospital-admissions-for-assault-by-sharp-object-february-2022
[35] V. Govender, “Homicide and near-miss homicide problem profile version 2.0,” College of Policing, Surrey, 2023
[36] “PHE evidence review of treatment outcomes,” [Online]. Available: https://assets.publishing.service.gov.uk/media/5a7f7f8ded915d74e622ad4a/PHE_Evidence_review_of_drug_treatment_outcomes.pdf
[37] “NICE national guideline 64,” [Online]. Available: https://www.nice.org.uk/guidance/ng64
[38] “NICE clinical guideline 52,” [Online]. Available: https://www.nice.org.uk/guidance/CG52
[39] “NICE clinical guideline 51,” [Online]. Available: https://www.nice.org.uk/guidance/CG51
[40] “NICE national guideline 58,” [Online]. Available: https://www.nice.org.uk/guidance/ng58
[41] “NICE quality standard 23,” [Online]. Available: https://www.nice.org.uk/guidance/qs23
[42] “NICE clinical guideline 115,” [Online]. Available: https://www.nice.org.uk/guidance/cg115
[43] “NICE guidance PH24,” [Online]. Available: https://www.nice.org.uk/guidance/ph24
[44] “NICE clinical guideline 100,” [Online]. Available: https://www.nice.org.uk/guidance/cg100
[45] “OHID Alcohol and dug misuse prevention and treatment guidance,” [Online]. Available: https://www.gov.uk/government/collections/alcohol-and-drug-misuse-prevention-and-treatment-guidance
[46] “OHID drug misuse and dependence guidelines on clinical management,” [Online]. Available: https://www.gov.uk/government/publications/drug-misuse-and-dependence-uk-guidelines-on-clinical-management
[47] “Service user involvement: a guide,” [Online]. Available: https://assets.publishing.service.gov.uk/media/5a82ed36ed915d74e6238547/Service-user-involvement-a-guide-for-drug-and-alcohol-commissioners-providers-and-service-users.pdf
[48] “PHE NPS toolkit,” [Online]. Available: https://assets.publishing.service.gov.uk/media/5a82ee39e5274a2e87dc3b1e/9011-phe-nps-toolkit-update-final.pdf
[49] “Substance misuse services for men involved in chemsex,” [Online]. Available: https://www.gov.uk/government/publications/substance-misuse-services-for-men-involved-in-chemsex
[50] “Hard Edges,” [Online]. Available: https://lankellychase.org.uk/publication/hard-edges/
[51] “Changing Futures – Bridge the Gap,” [Online]. Available: https://www.healthysurrey.org.uk/community-health/changing-futures#bridgethegap
[52] “Pharmacy closures supplementary statement,” [Online]. Available: https://www.surreyi.gov.uk/dataset/2nron/pharmacy-closures-supplementary-statement-to-the-surrey-pharmaceutical-needs-assessment-june-2023
[53] “OHID Alcohol and drug treatment in secure settings,” [Online]. Available: https://www.gov.uk/government/statistics/substance-misuse-treatment-in-secure-settings-2021-to-2022/alcohol-and-drug-treatment-in-secure-settings-2021-to-2022-report
[54] “Surrey County Council census 2021 ethnic group,” [Online]. Available: https://www.surreyi.gov.uk/census-2021/ethnic-group/
[55] https://www.surreyi.gov.uk/jsna/surrey-context/#:~:text=Of%20Surrey%27s%20population%3A,Elmbridge%20to%2016.5%25%20in%20Guildford [Online]
[56] “Health and wellbeing strategy: Healthy Surrey,” [Online]. Available: https://www.healthysurrey.org.uk/about/strategy
[57] “ONS drug misuse 2022,” [Online]. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/drugmisuseinenglandandwales/yearendingjune2022
[58] “Fingertips MH JSNA,” [Online]. Available: https://fingertips.phe.org.uk/profile-group/mental-health/profile/mh-jsna
[59] “OHID mental health profile CYPMH,” [Online]. Available: https://fingertips.phe.org.uk/profile-group/mental-health/profile/cypmh
[60] “Mental health of children and young people in England,” [Online]. Available: https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2023-wave-4-follow-up/data-sets
[61] “https://www.gov.uk/government/publications/specialist-drug-and-alcohol-services-for-young-people-a-cost-benefit-analysis,” [Online]. Available: https://www.gov.uk/government/publications/specialist-drug-and-alcohol-services-for-young-people-a-cost-benefit-analysis
[62] “OHID Co-occurring substance misuse and mental health issues” [Online]. Available: Co-occurring Substance Misuse and Mental Health Issues – OHID (phe.org.uk)